Session Ten: Blinding
This episode is a live recording of the ninth session of #UnblindingResearch held in DREEAM 19th December 2018. The group work has been removed for the sake of brevity.
This session of #UnblindingResearch looks at blinding, how we do it and when we can’t. Here are the slides for this session (p cubed of course), you can move between slides by clicking on the side of the picture or using the arrow keys.
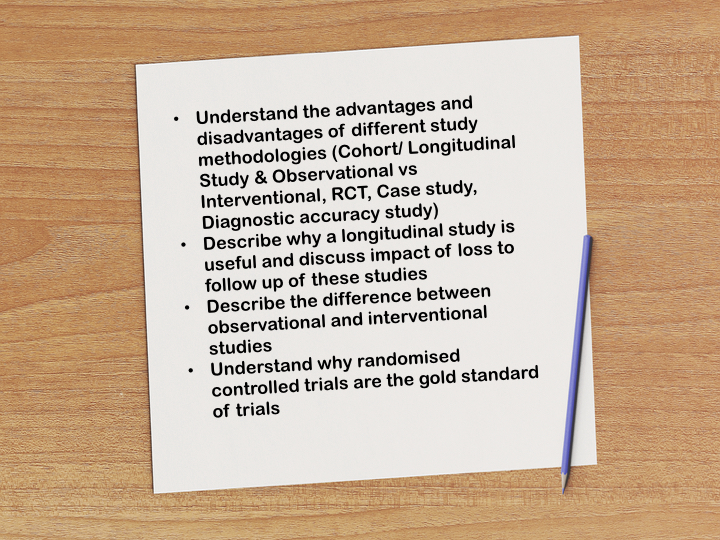
Blinding is the concealment of allocation from one or more person involved in the research process. Blinding is critical to randomised control trials. In the previous episode we discussed randomisation; a critical part of eliminating selection bias from recruitment and allocation. Blinding is involved after the randomisation process and reduces performance and ascertainment bias.
Performance bias refers to the difference in care provided to participants in a trial other than the treatment being compared. If a patient knows they receiving a potential new treatment they are more likely to report placebo effects and exaggerate any benefits. Healthcare workers involved in the trial may provide different standards of care if they know a certain patient is receiving the new treatment or the placebo. If a patient knows they are receiving placebo this may affect their engagement with the study or make them seek other care as well and affect internal validity.
Ascertainment bias refers to the tendency to look harder for results if you know a patient has had the intervention/new treatment. If a patient was known to be on your new treatment they are likely to have more intense surveillance for any potential benefits rather than the control/placebo arm which are likely to be ignored.
There is no analytical method to correct any performance or ascertainment bias and so we must be VERY careful when reading an unblinded trial.
In most RCTs there are broadly 3 groups of people involved: patients, clinicians/data collectors and data analysts.
In single blind trials the patient doesn’t know their allocation but everyone else does.
In double blind trials neither the patient or their clinician/data collector know the allocation but the data analyst will.
In triple blind trials even the data analyst is blinded from allocation which is only revealed once results have been written up.
But not every trial can be blinded. Cohort studies, for example, are difficult to blind as patients tend to know if they have a certain condition as part of being included in the study. Surgical trials are difficult to blind as patients will know if they have had surgery to the presence of scars afterwards. Trials involving surgery therefore tend to use expertise-based design where patients are allocated to one of several surgeons who each perform one kind of surgery.
Other tactics for studies where blinding is not possible include:
standardisation as much as possible of all processes leaving the allocation as the only variable
only recording objective and reliable outcomes
duplicate assessments if possible
acknowledge limitations of the study
Here is the #TakeVisually for this episode: