Heart Murmurs
Senior ACP in Emergency Medicine Ru Thow makes his pod debut to discuss Heart Murmurs! We cover Aortic Regurgitation, Aortic Stenosis, Mitral Regurgitation and Mitral Stenosis. Features examples of these murmurs. We've also released separate podcasts containing just the murmurs!
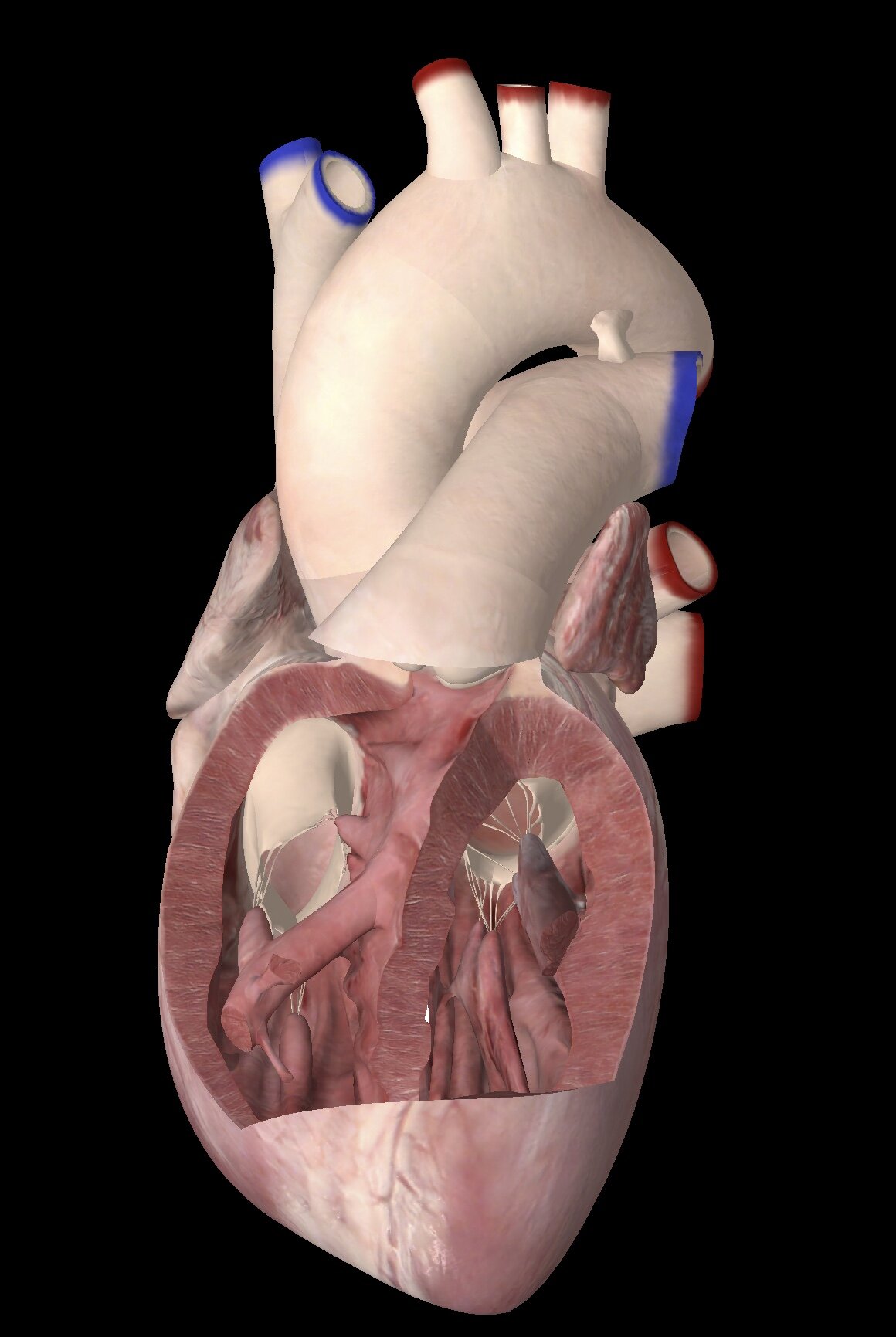
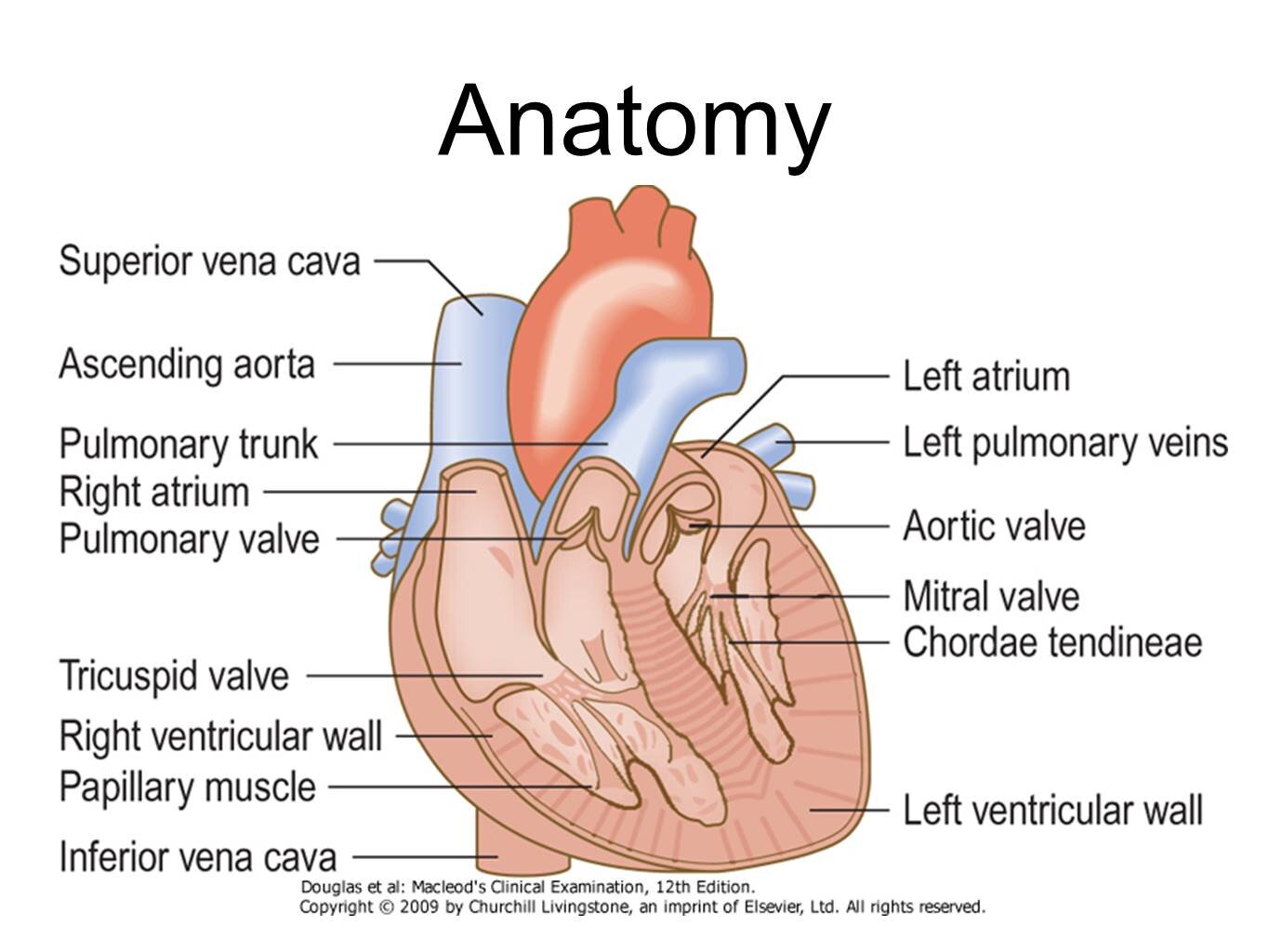
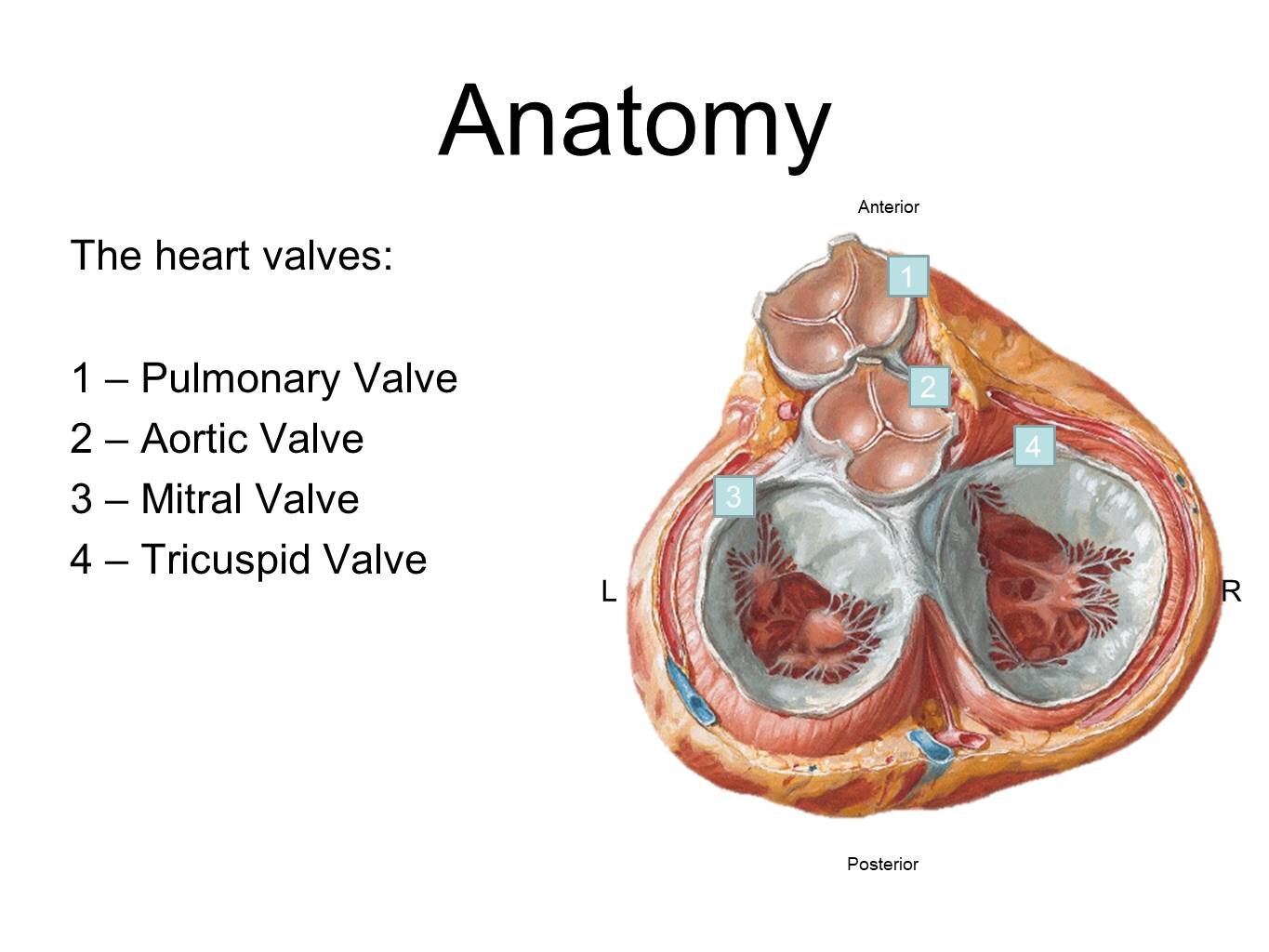
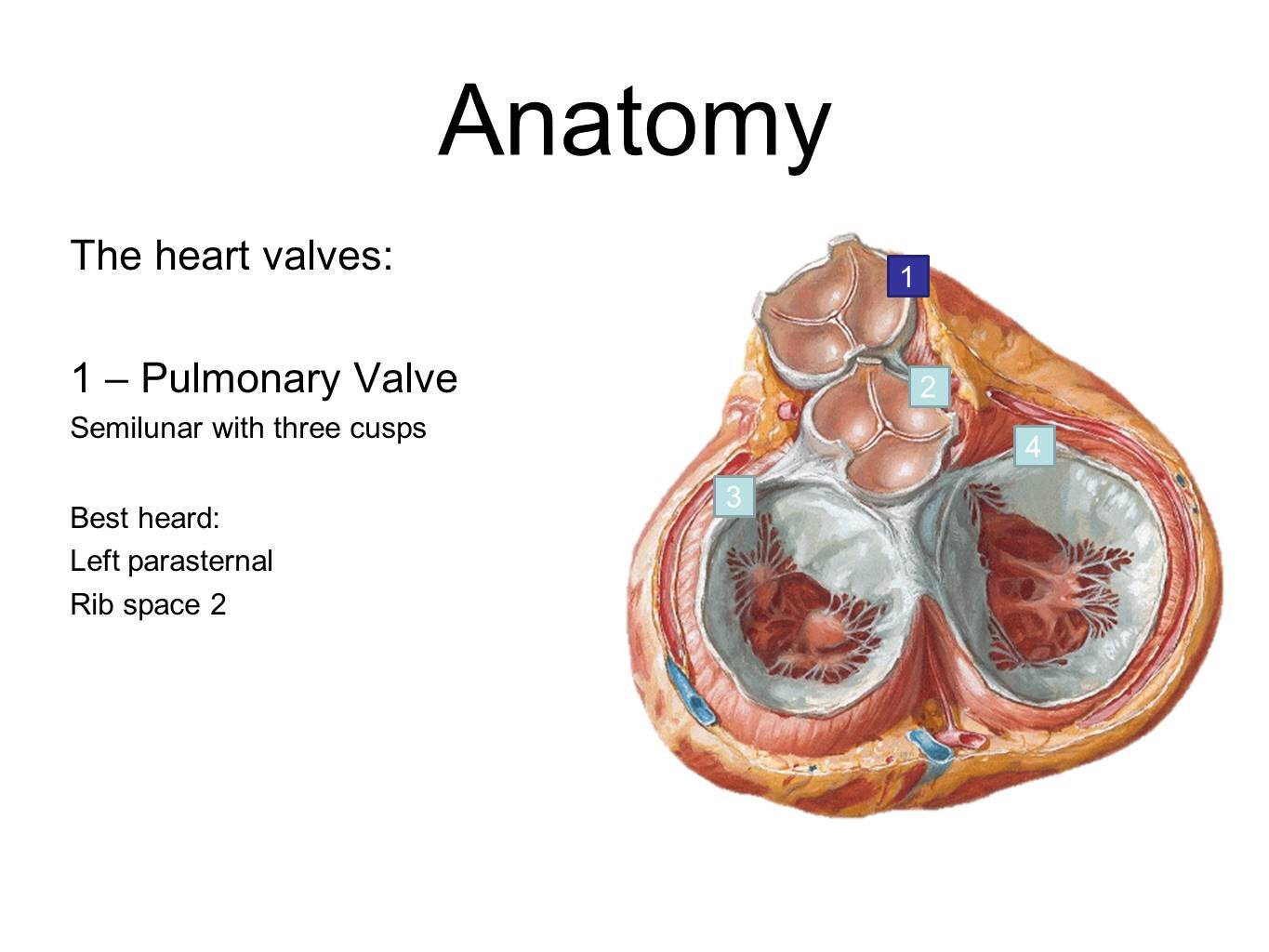
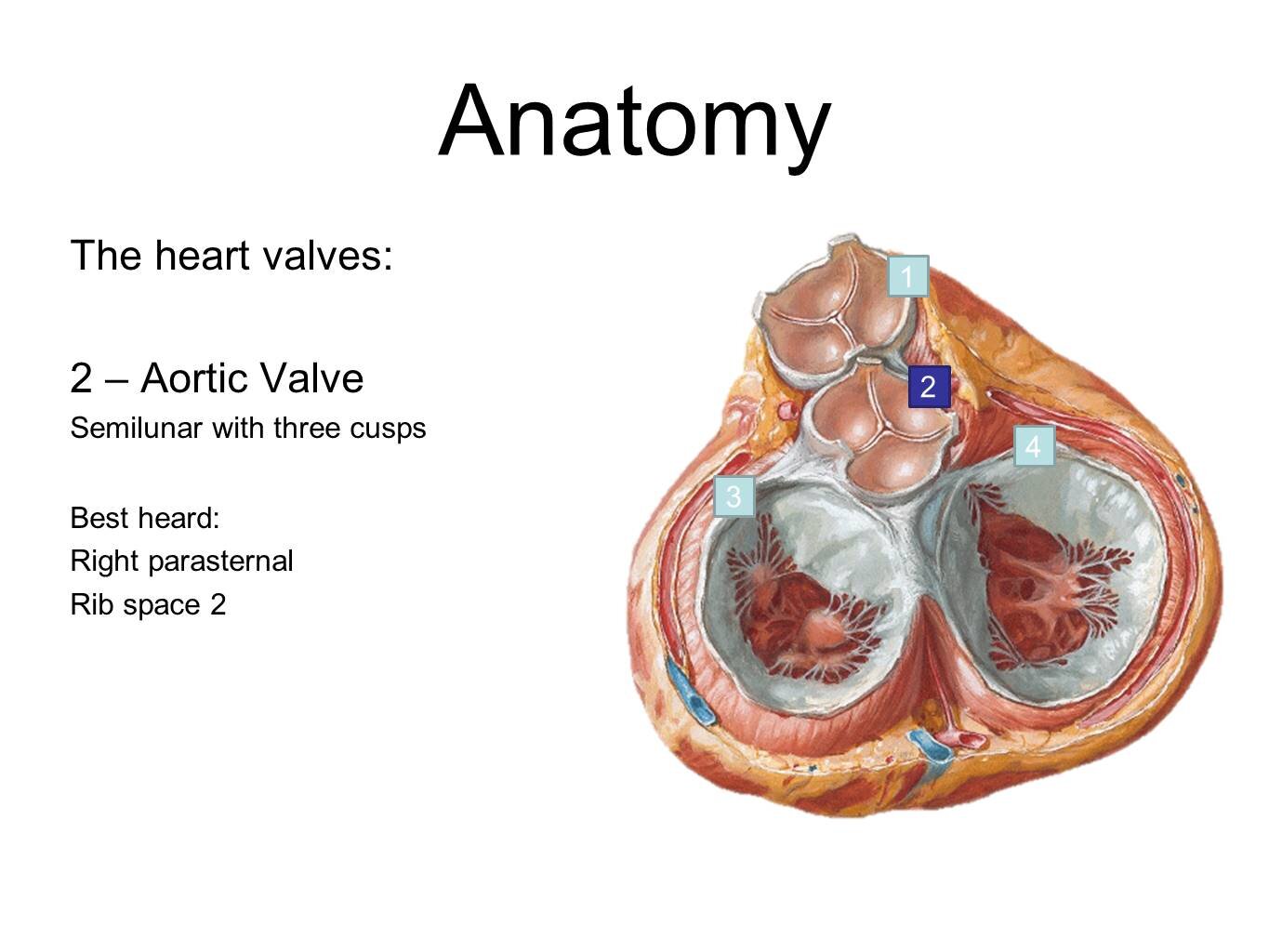
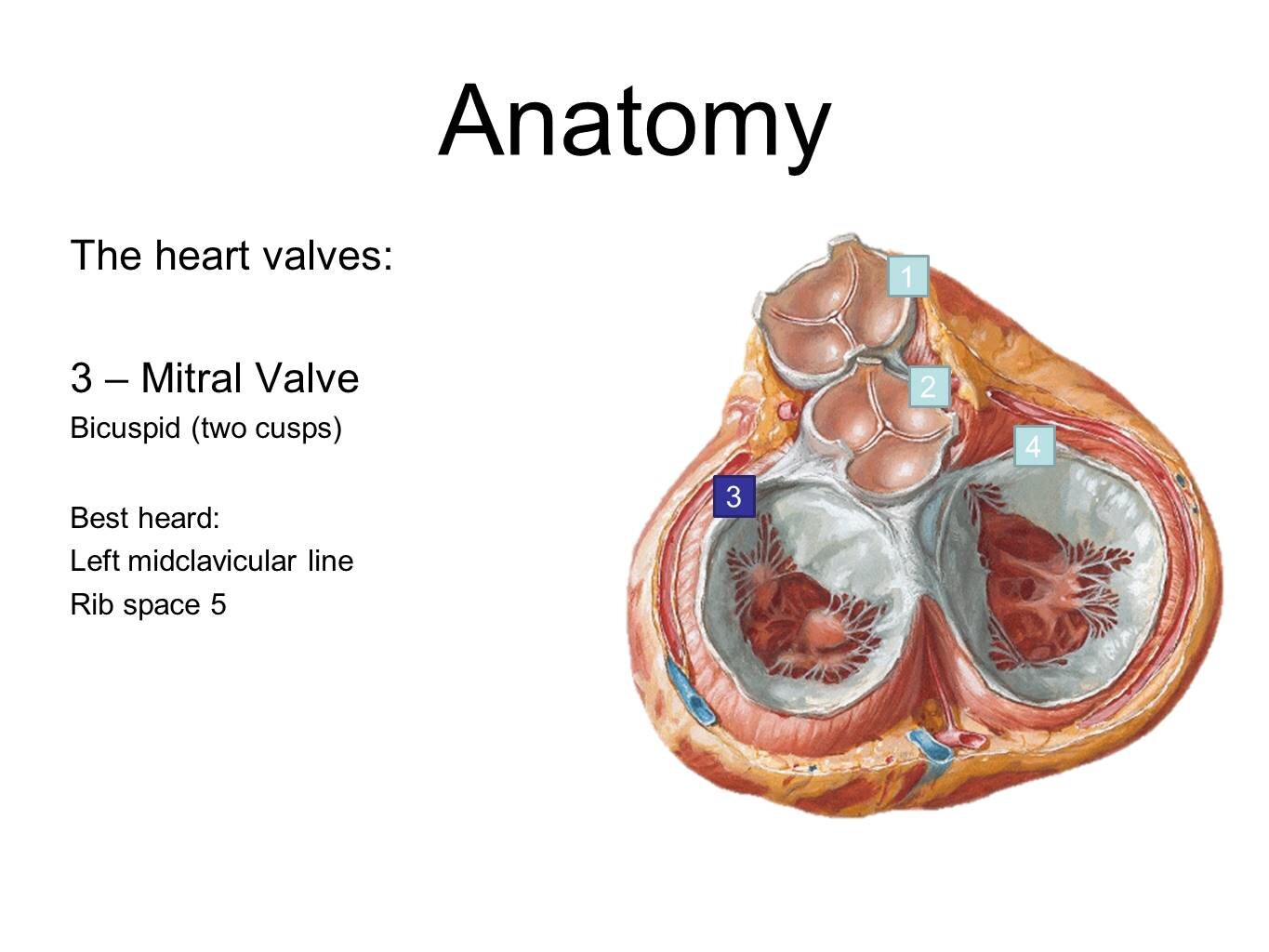
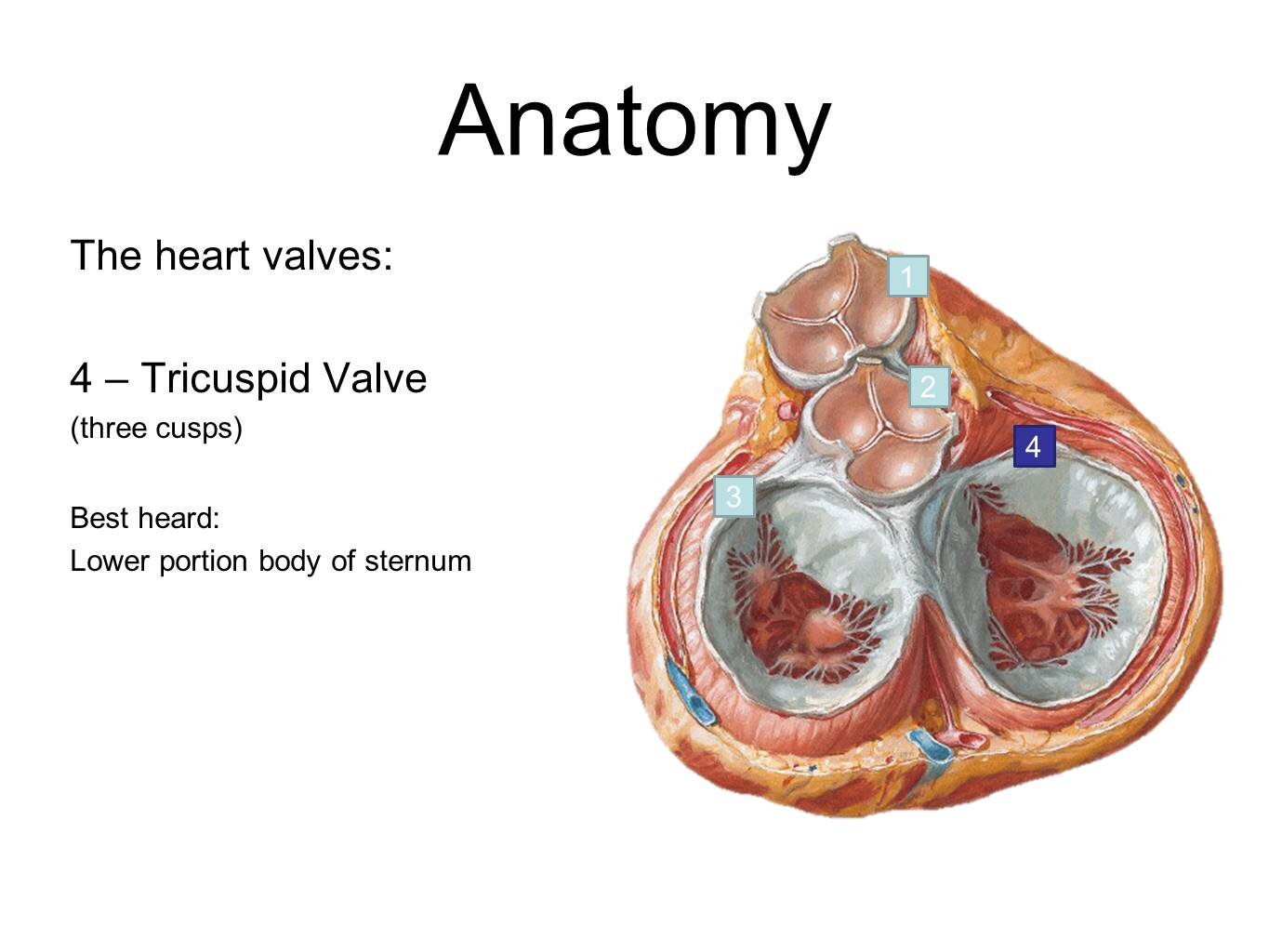
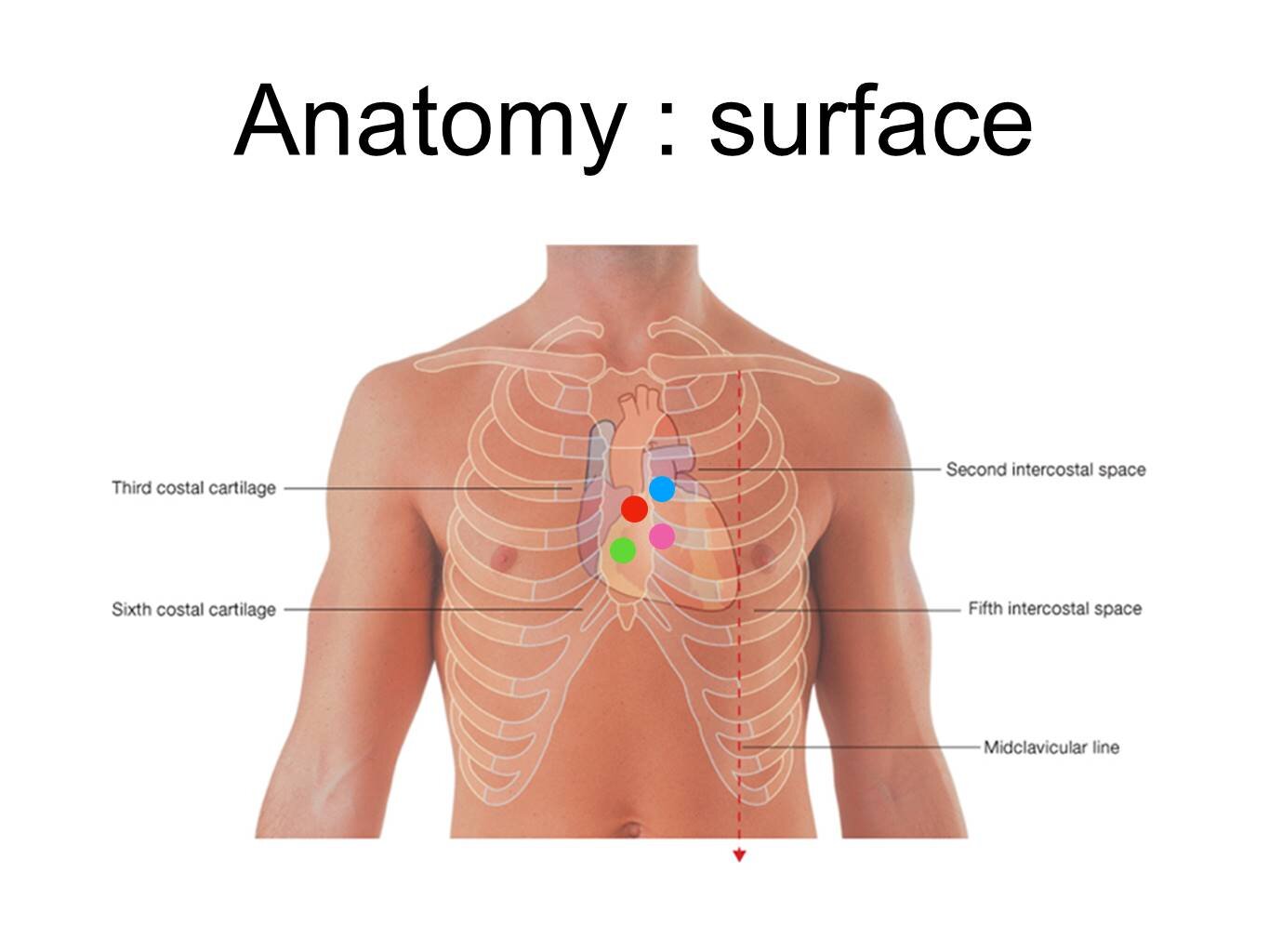
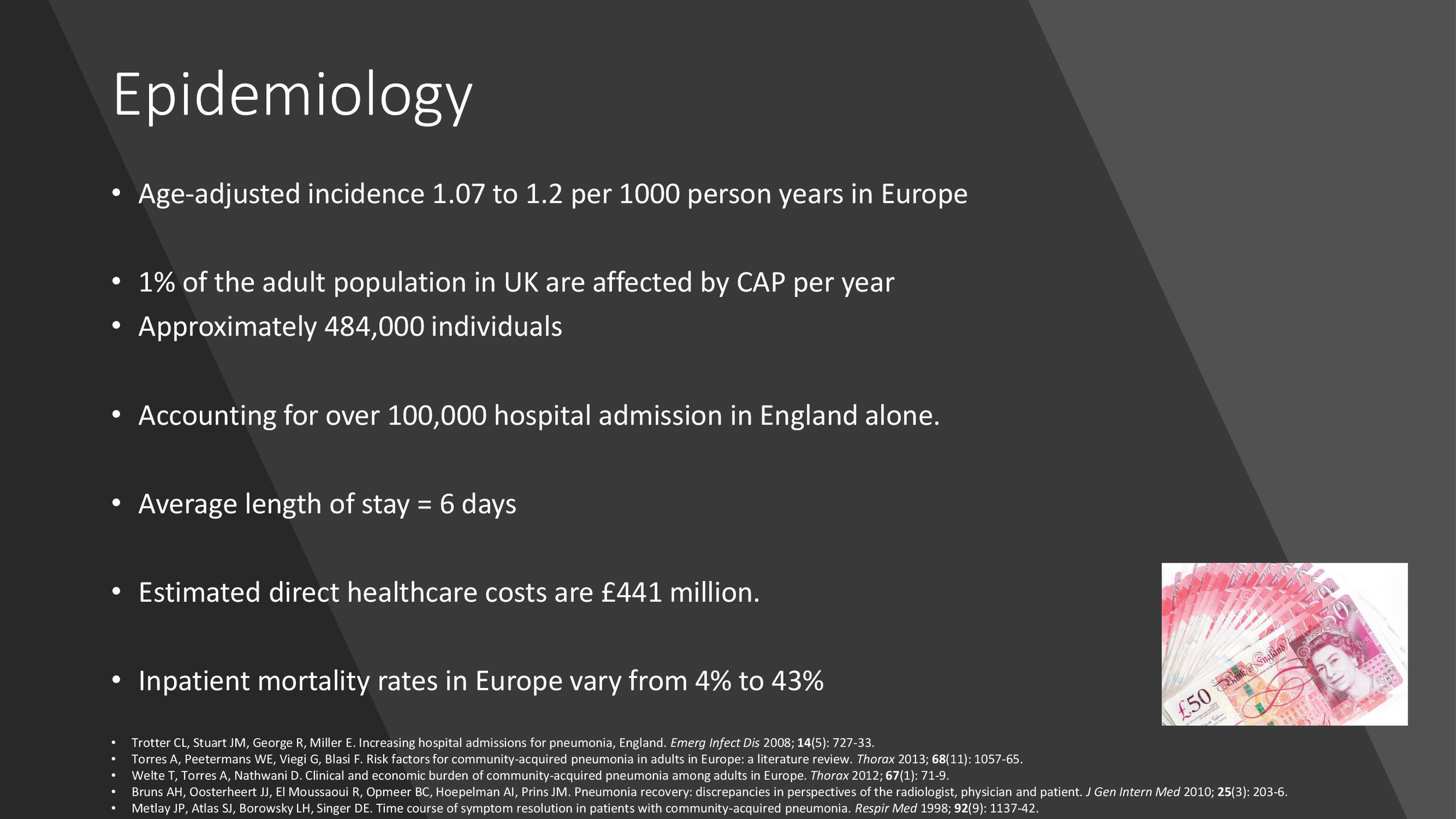
Pictures from Essential Anatomy application revealing the heart valves.
Here are Ru’s slide sets detailing murmur pathophysiology:
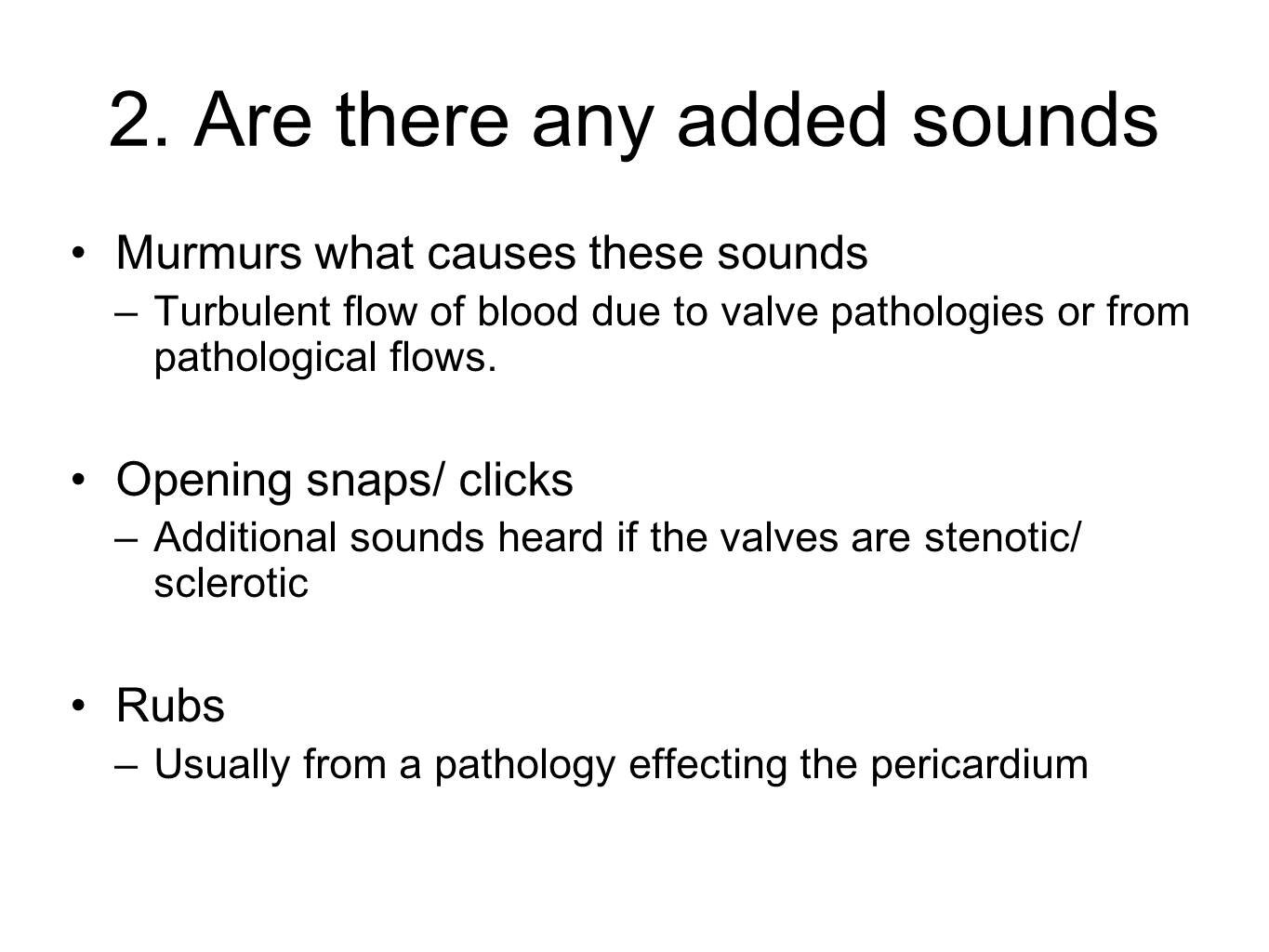
Blood flow should be laminar (all in the same direction). A murmur is caused by turbulent flow (something stopping the blow flowing in the same direction).
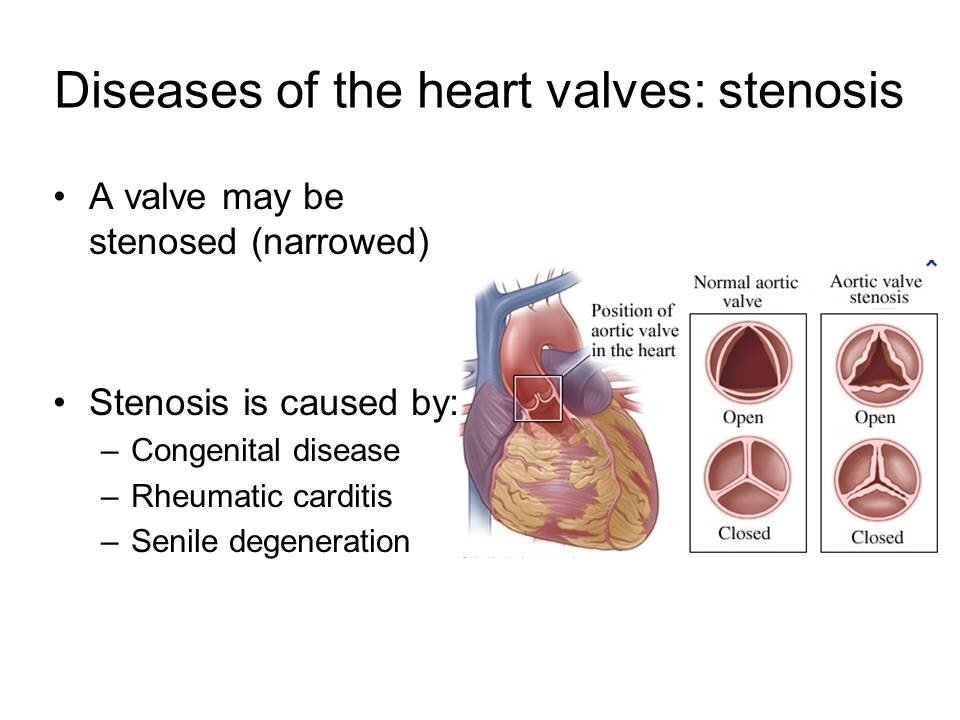
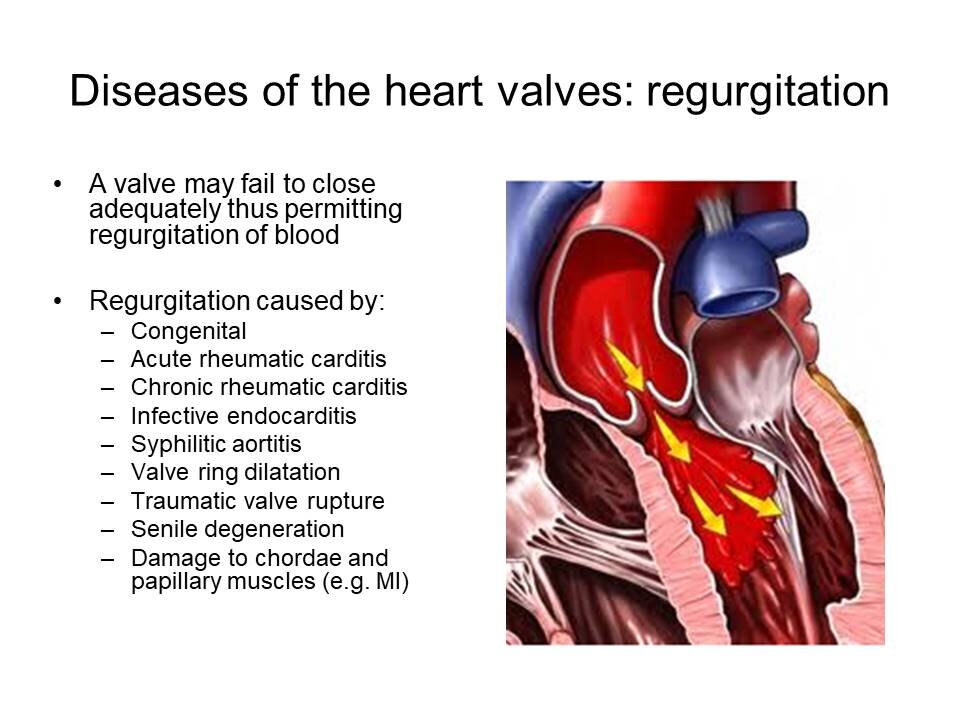
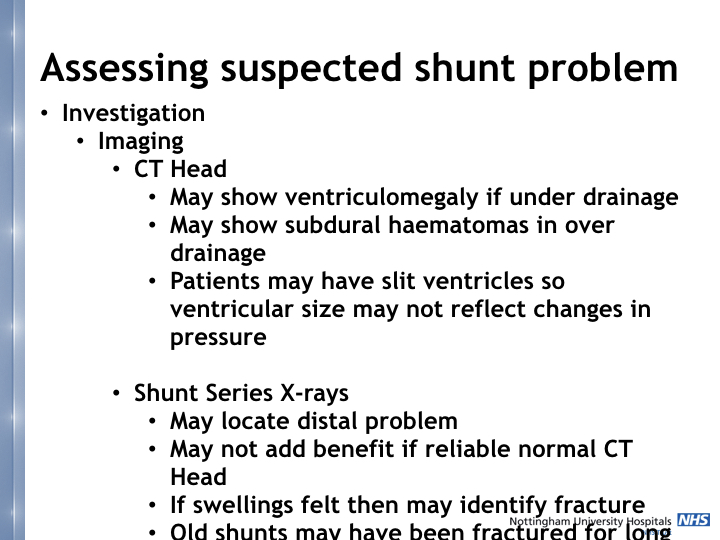
When it comes to valves two main types of disease cause them to make a murmur:
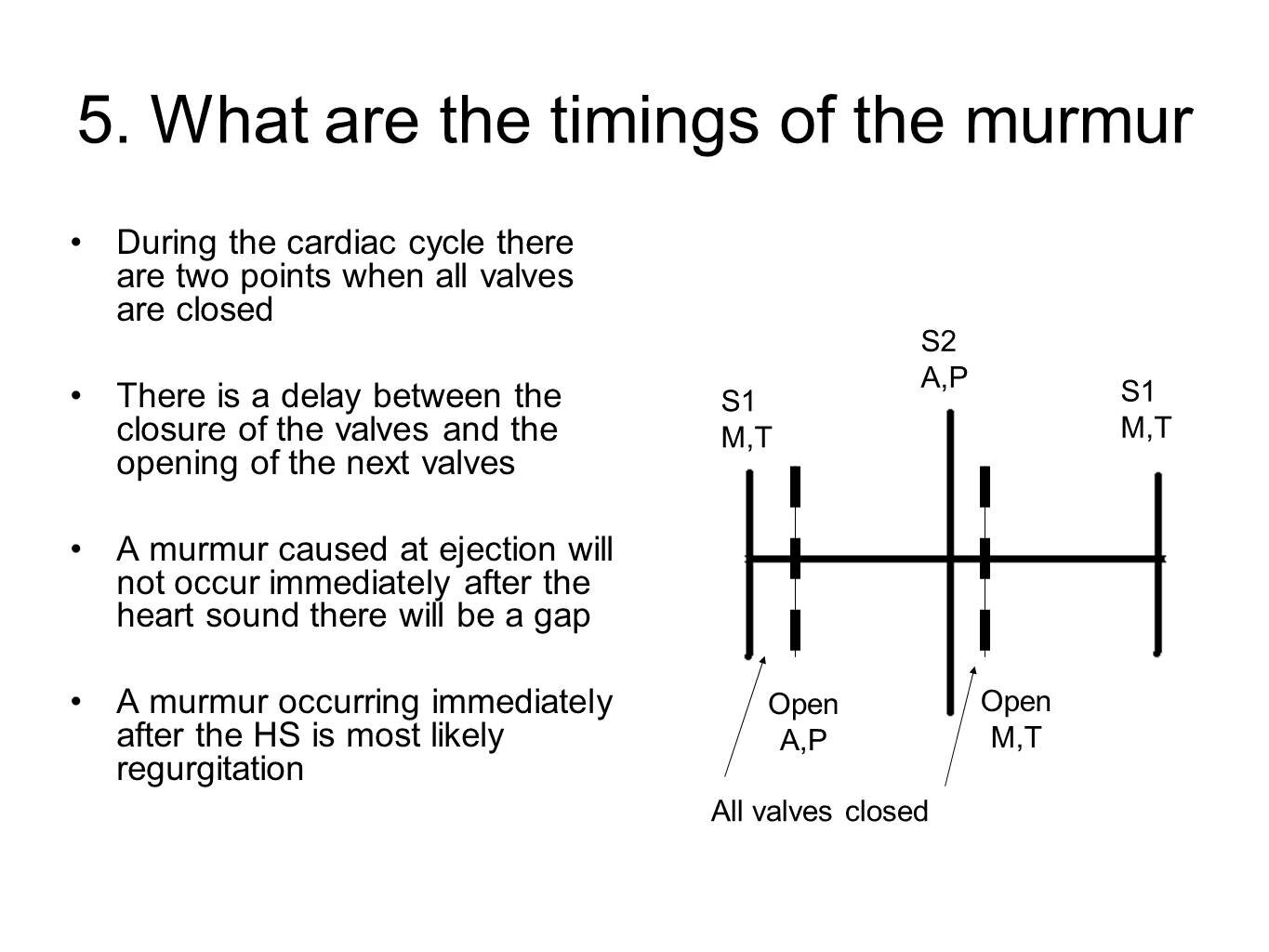
Stenosis: narrowing of valve, the murmur will be heard as the valves close
Regurgitation: caused by backflow of blood through a valve which has closed but is ‘leaking’, the murmur will be heard after the valve has closed
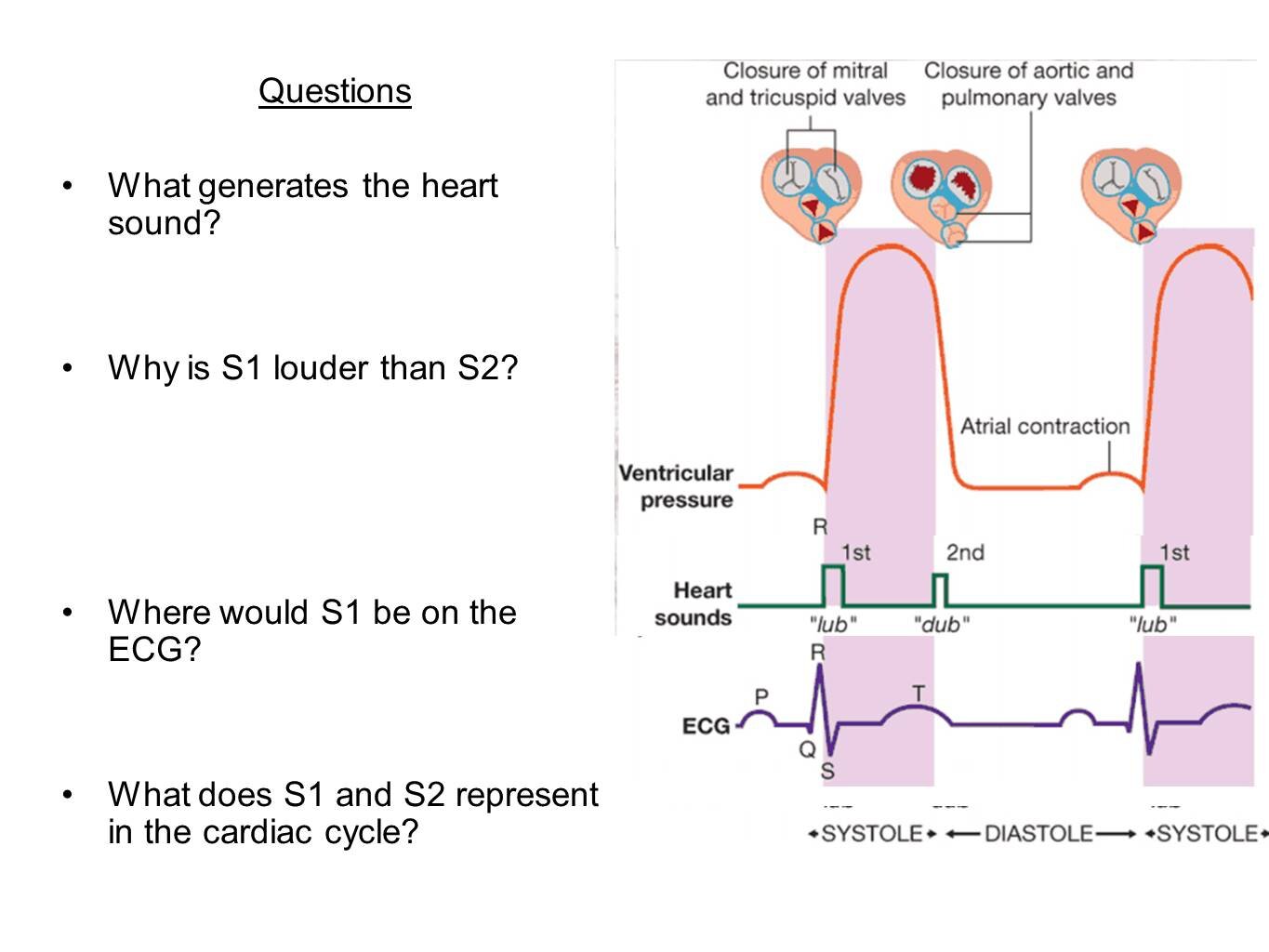
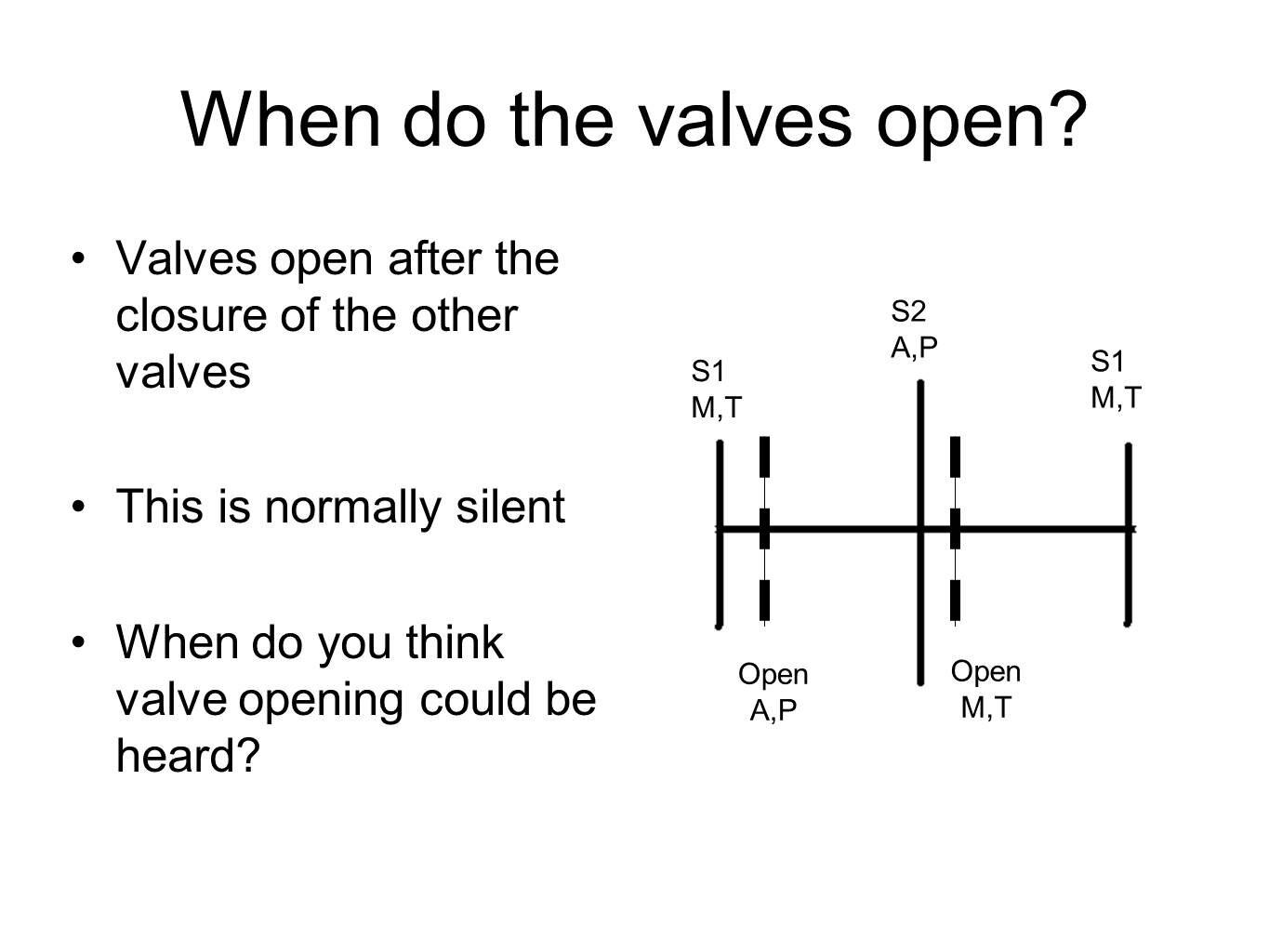
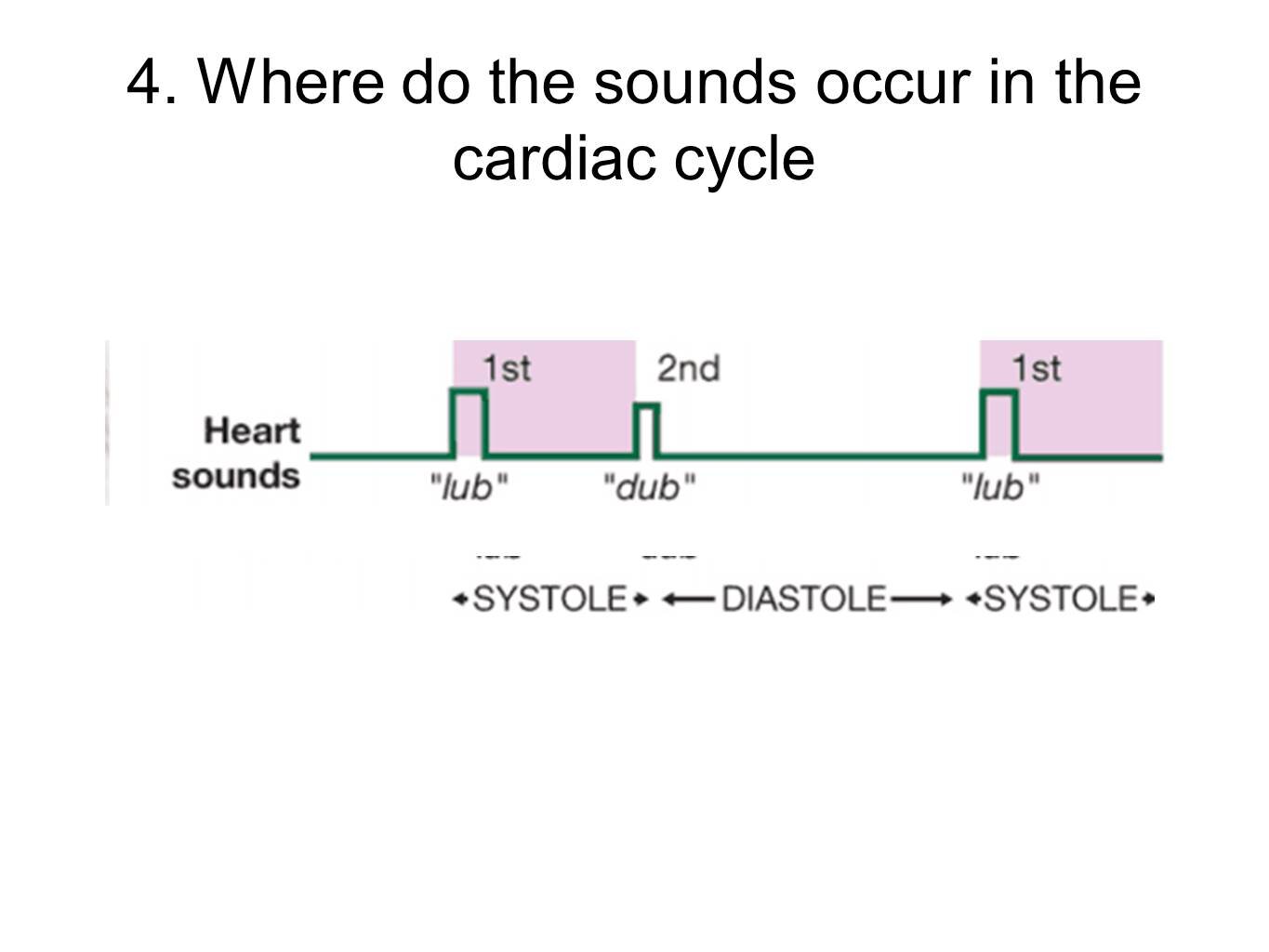
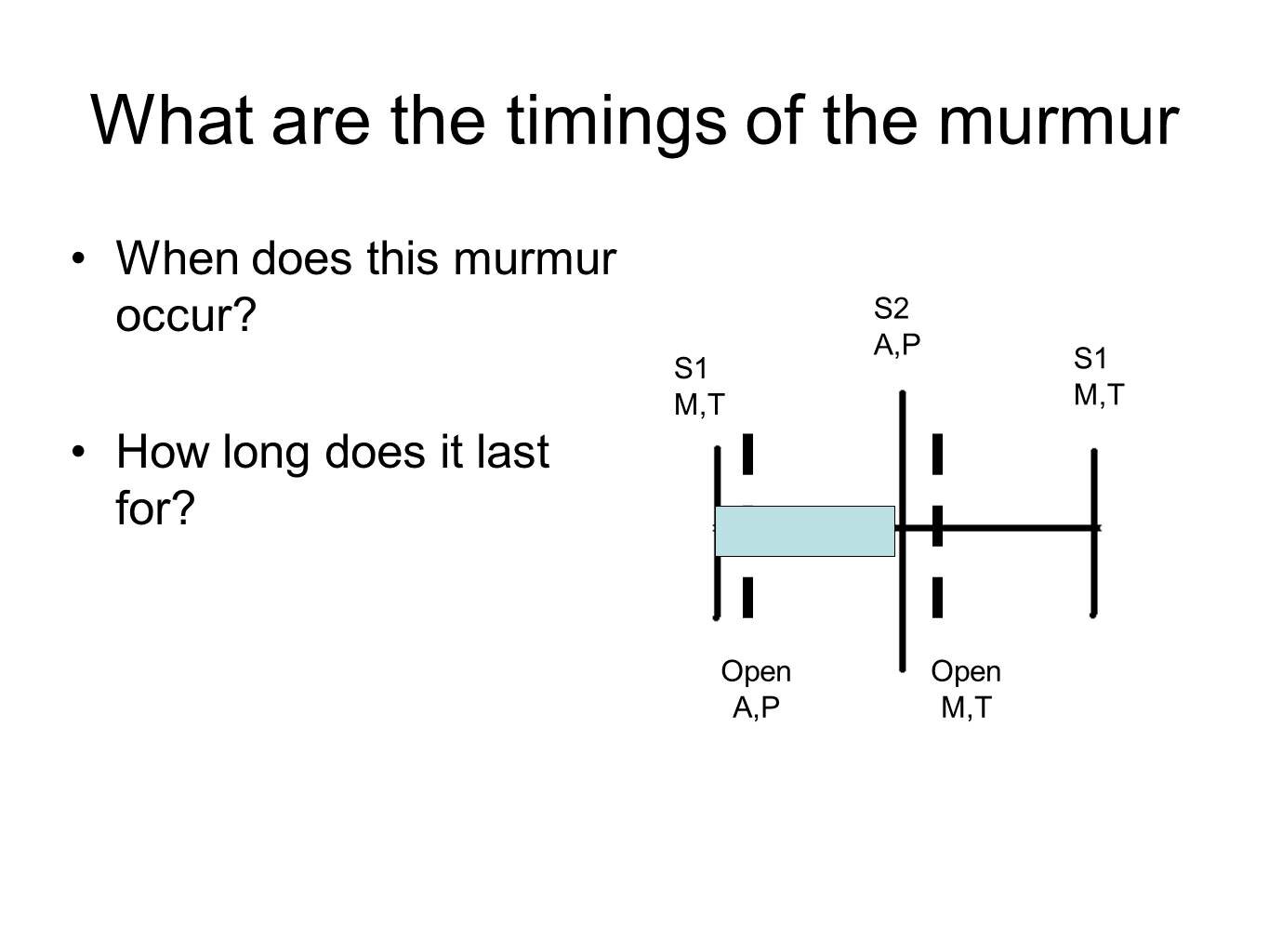
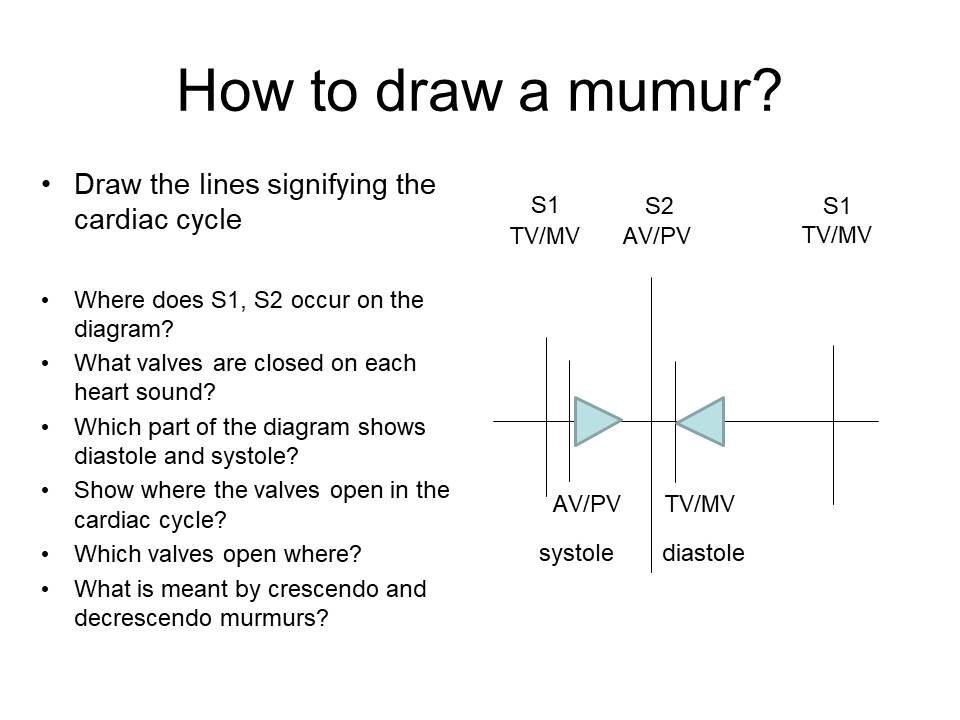
Normally there are two heart sounds, lub and dub
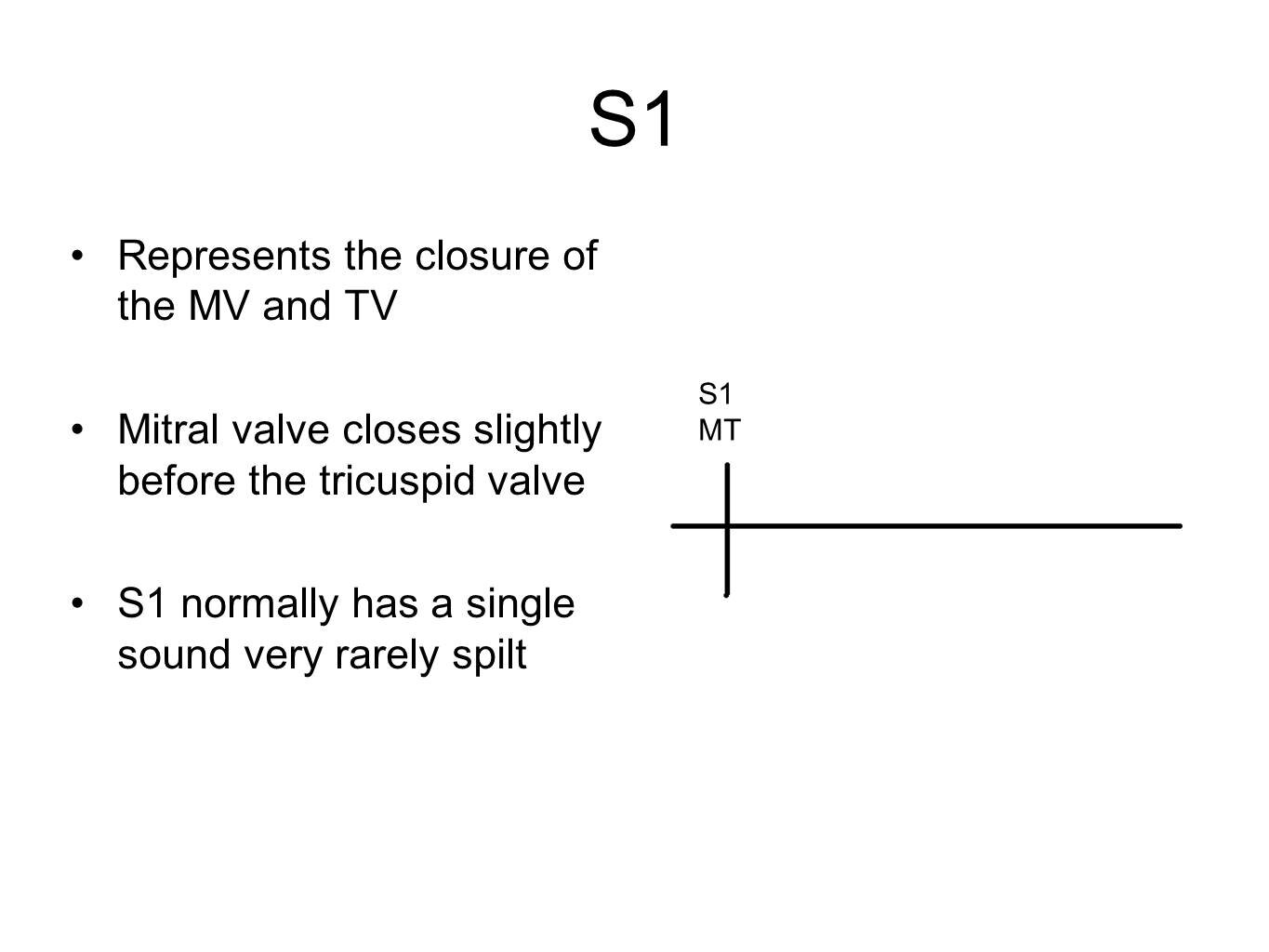
S1 (lub)
The start of systole
Made by the mitral and tricuspid valves closing to prevent backflow in atria
Aortic and pulmonary valves open to allow blood through them into aorta and pulmonary artery respectively
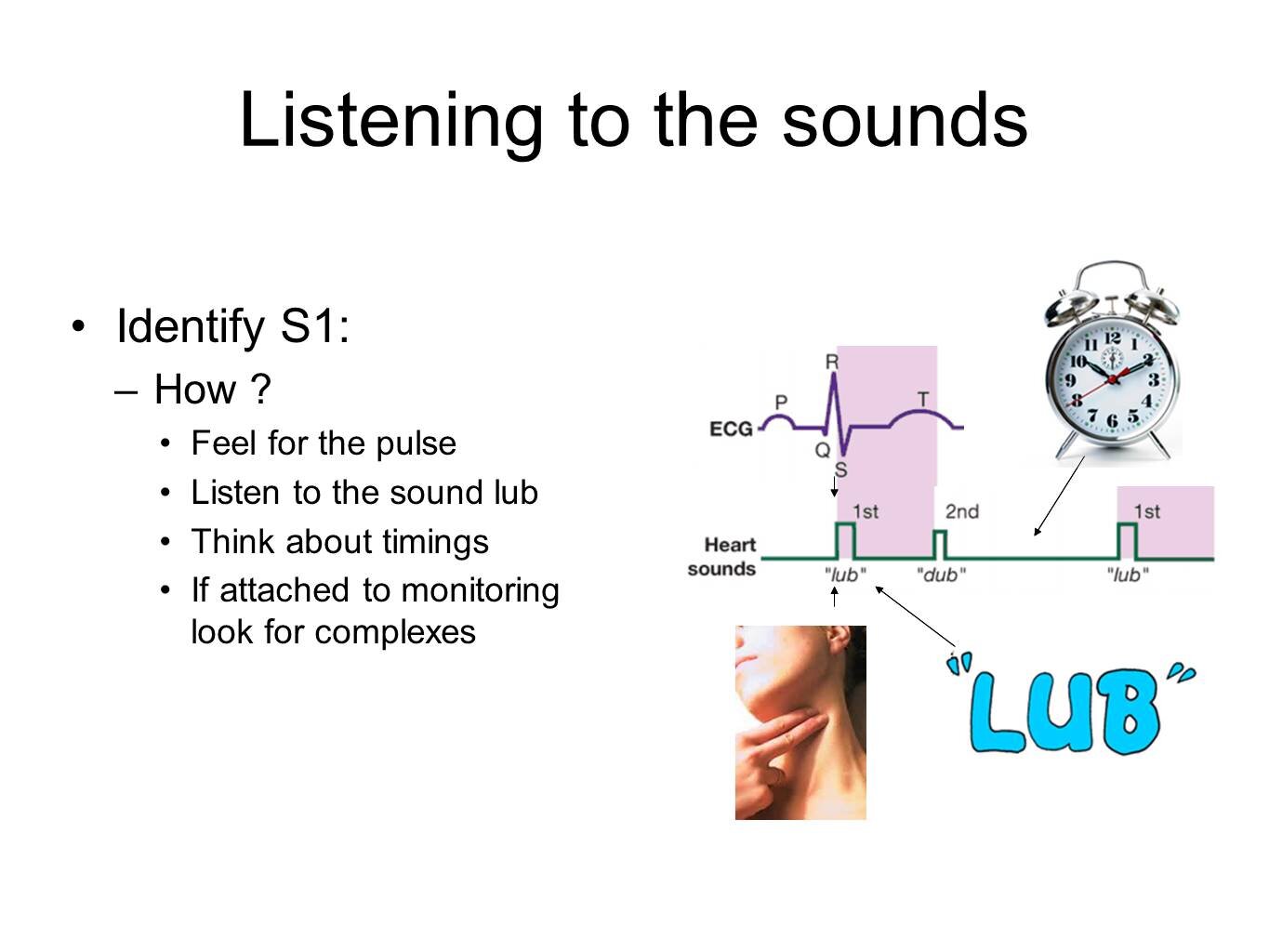
Corresponds to pulse
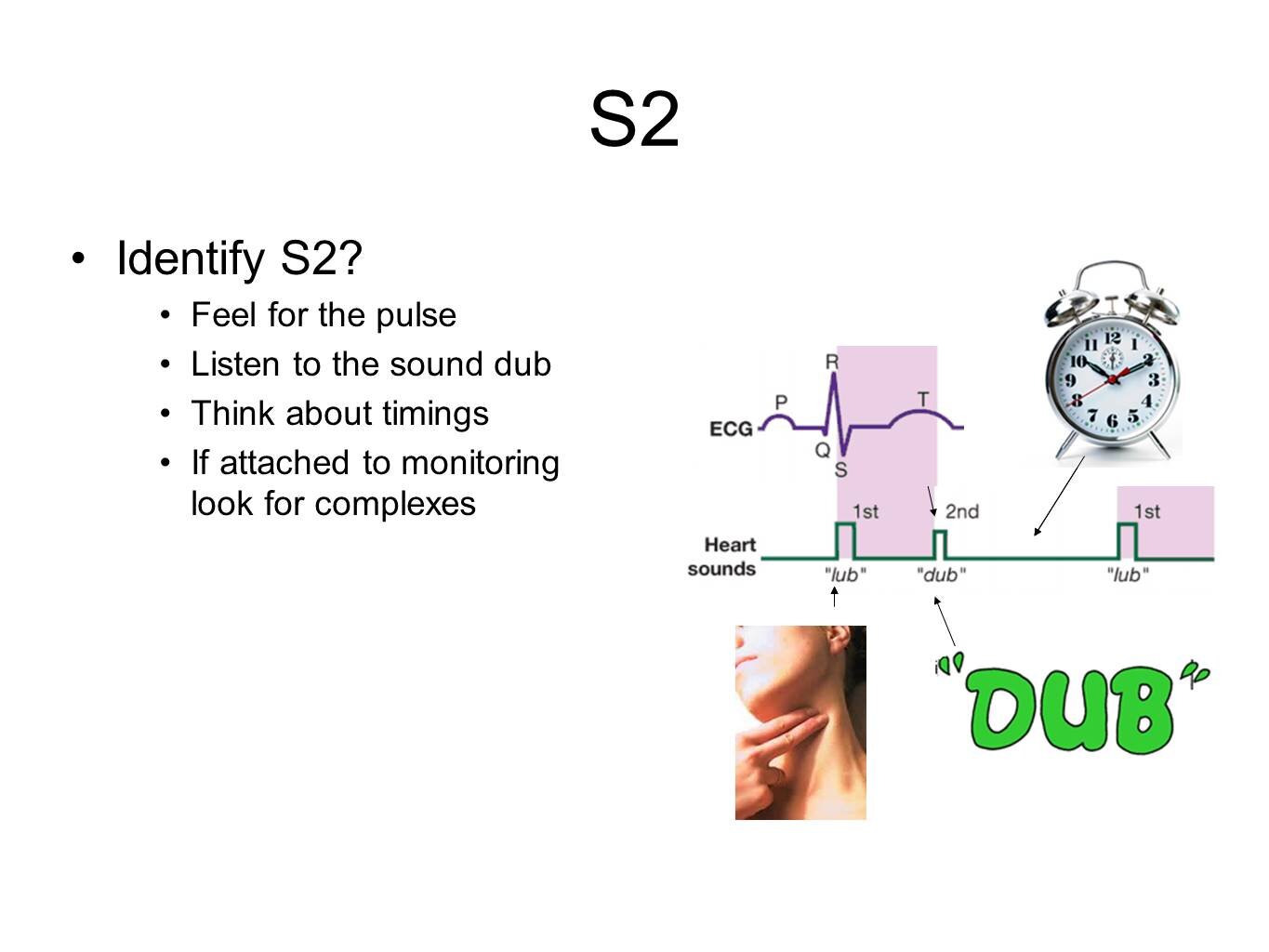
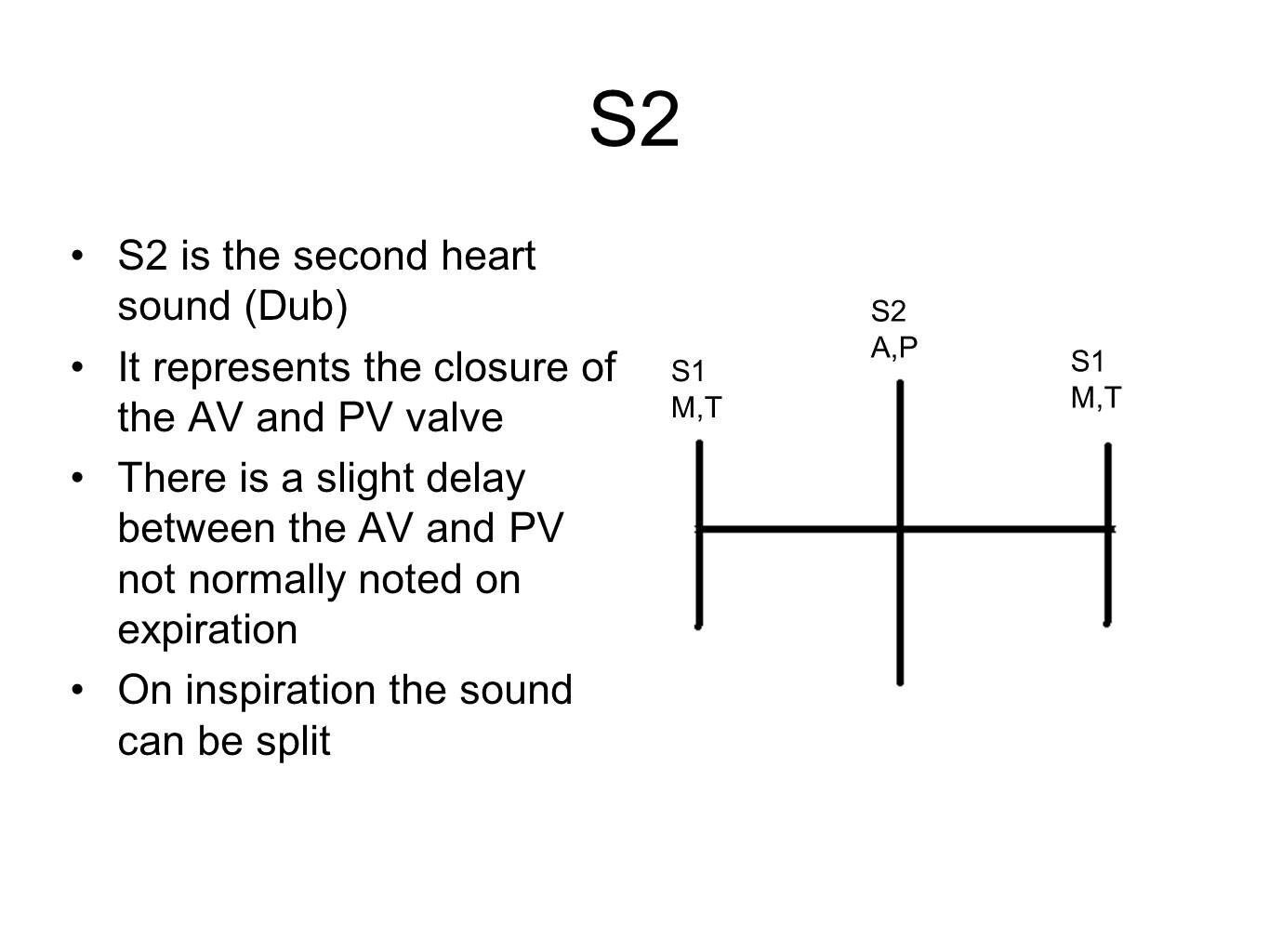
S2 (dub)
The end of systole and start of diastole
Made by the aortic and pulmonary valves closing to prevent backflow into ventricles
Mitral and tricuspid valves open to allow blood into ventricles
S1 (lub) - The sound which matches the pulse
Systole: the time between S1 and S2
Diastole: the time between S2 and S1
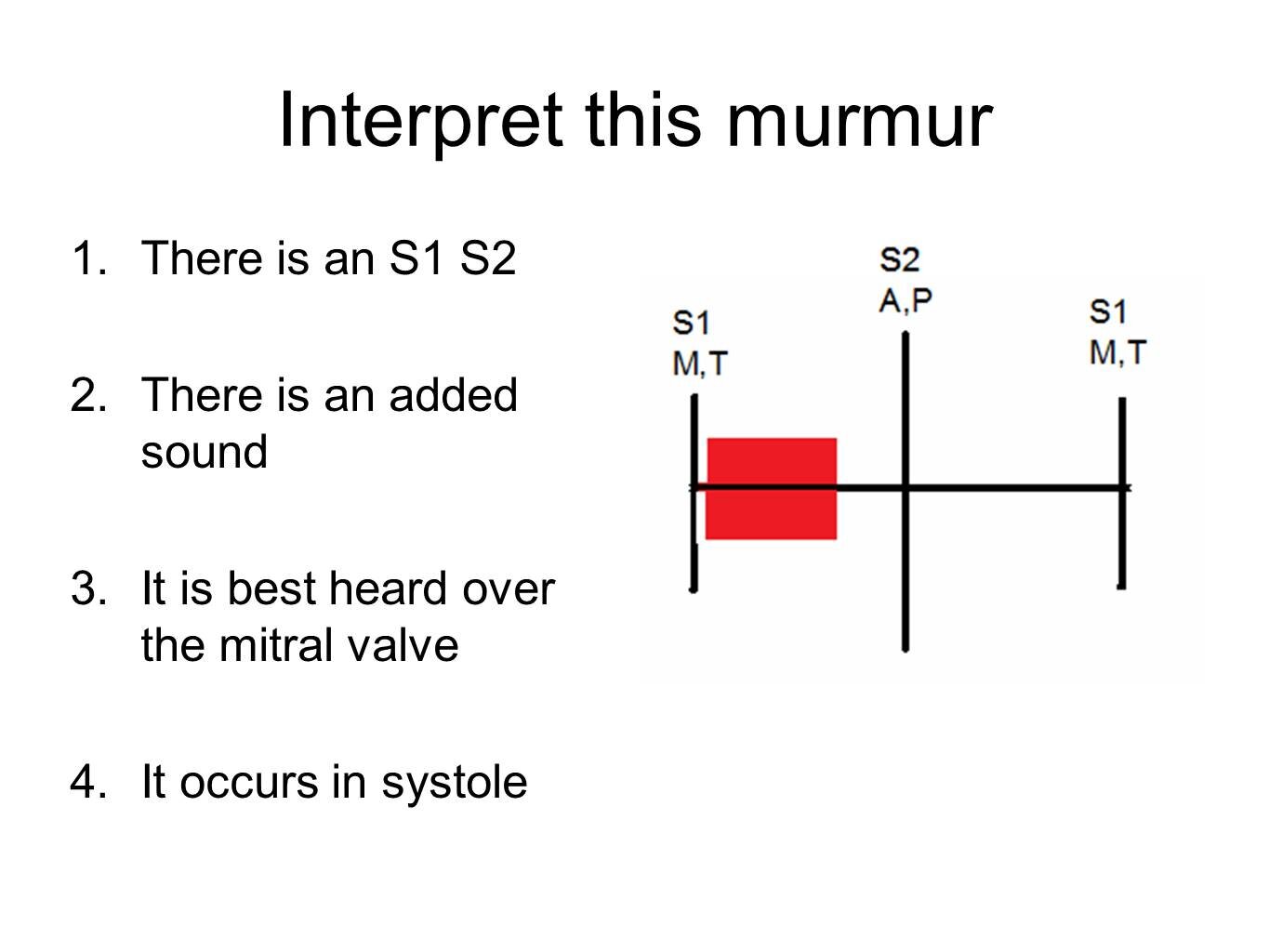
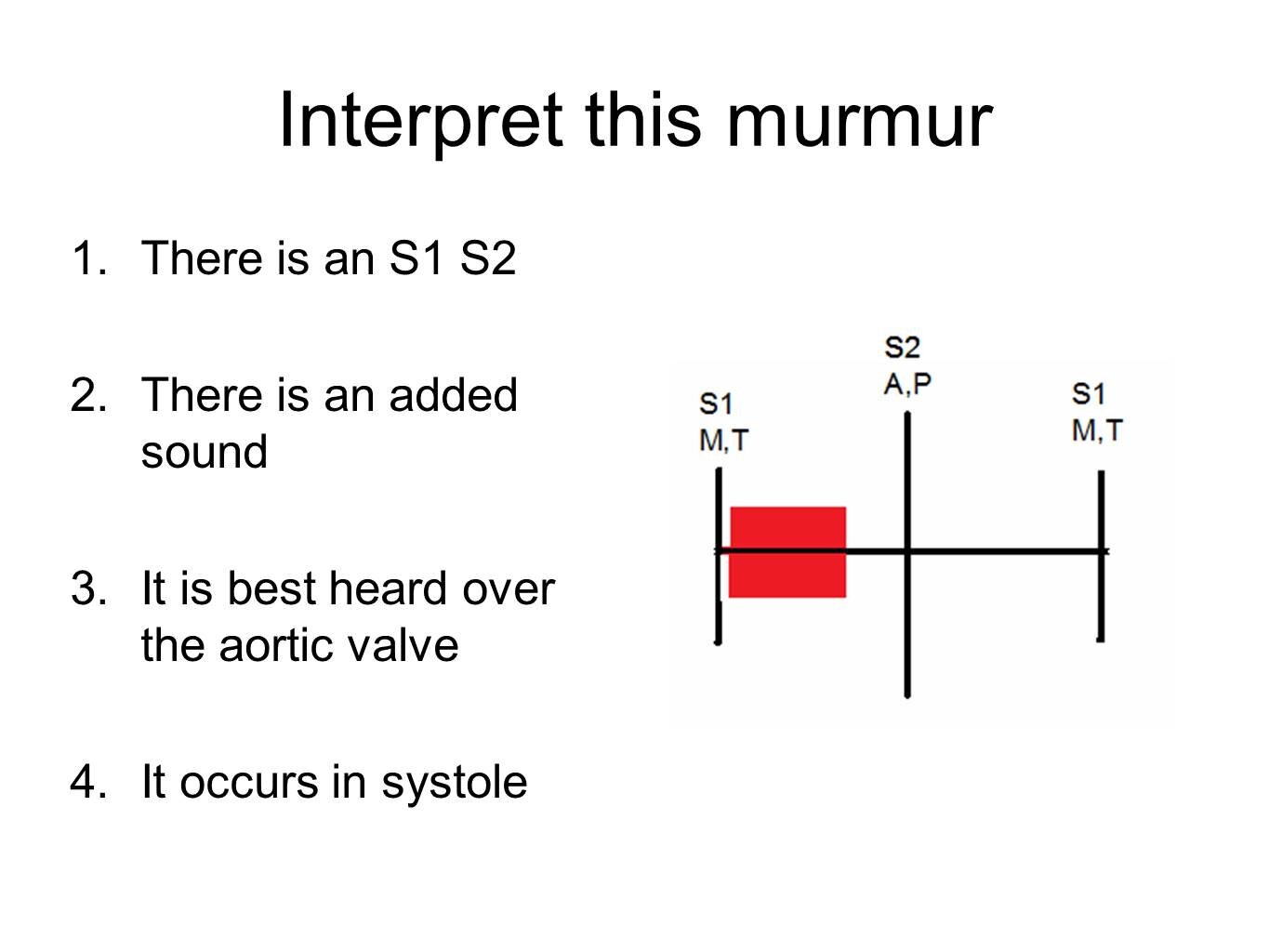
So in systole the mitral and pulmonary valves should be closed with blood flowing through the aortic and pulmonary valves. If the mitral valve is allowing a backflow you will hear this murmur in systole. If the aortic valve is narrowed you will hear this murmur in systole.
Mitral regurgitation and aortic stenosis are therefore systolic murmurs.
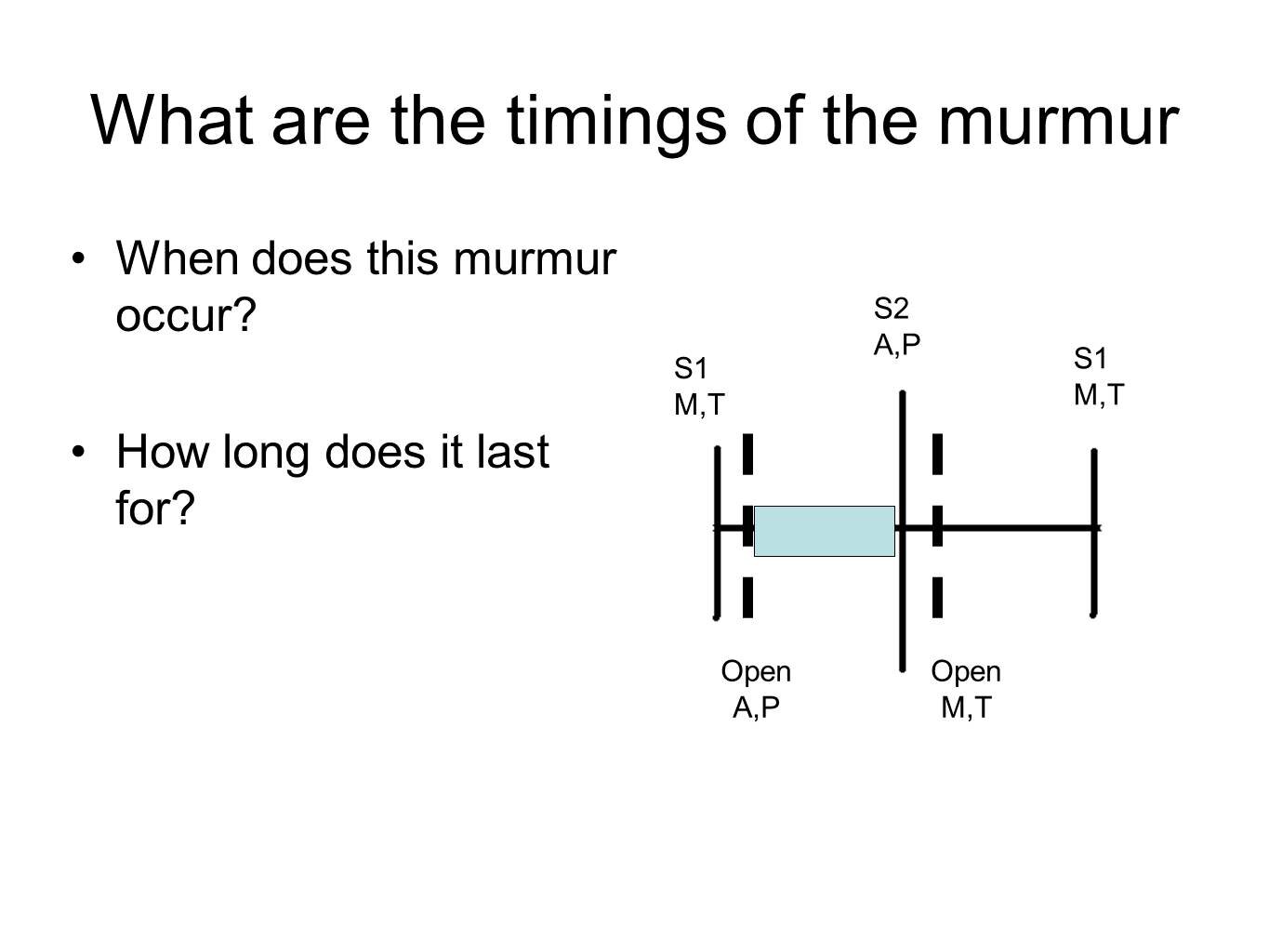
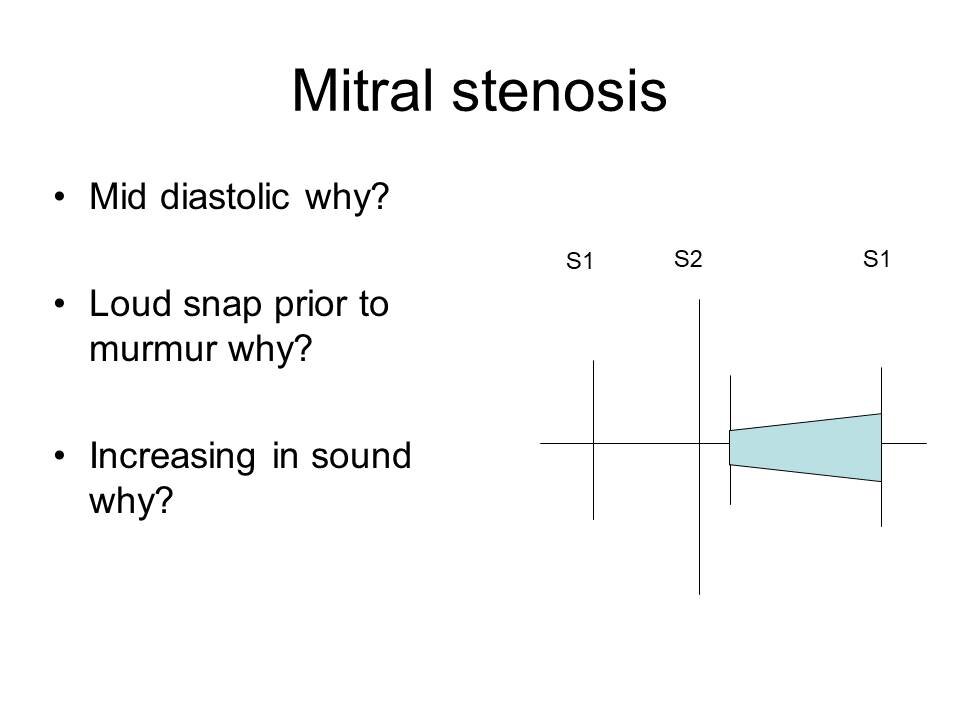
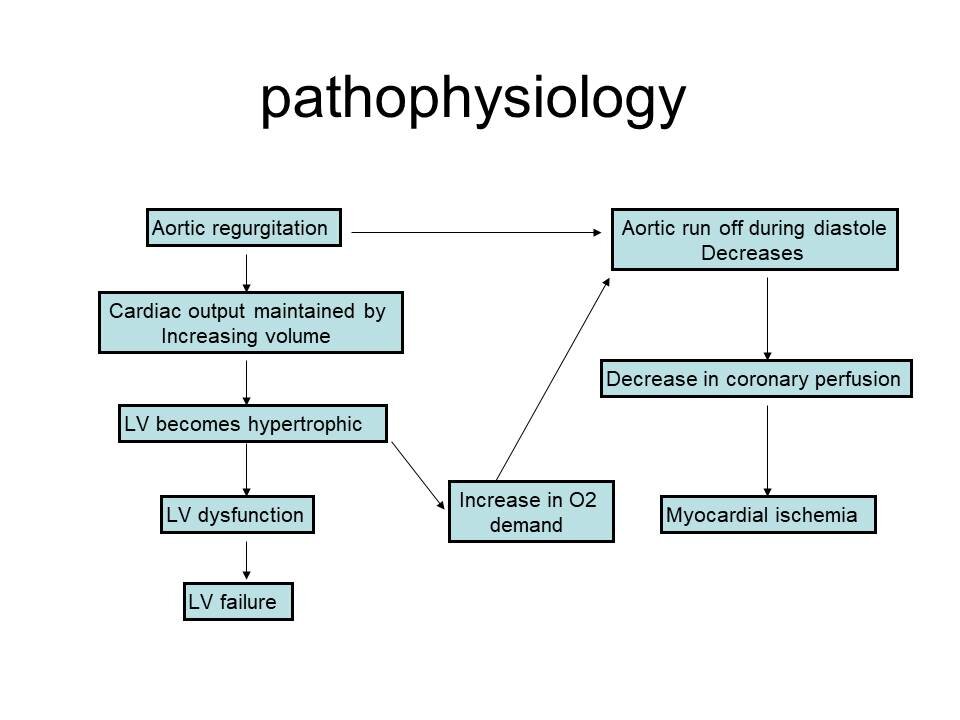
In diastole the mitral and tricuspid valves should be open with blood flowing into the ventricles with closed aortic and pulmonary valves. If the mitral valve is narrow you will hear this murmur in diastole. If the aortic valve is allowing a backflow of blood from the aorta into the left ventricle you will hear this murmur in diastole.
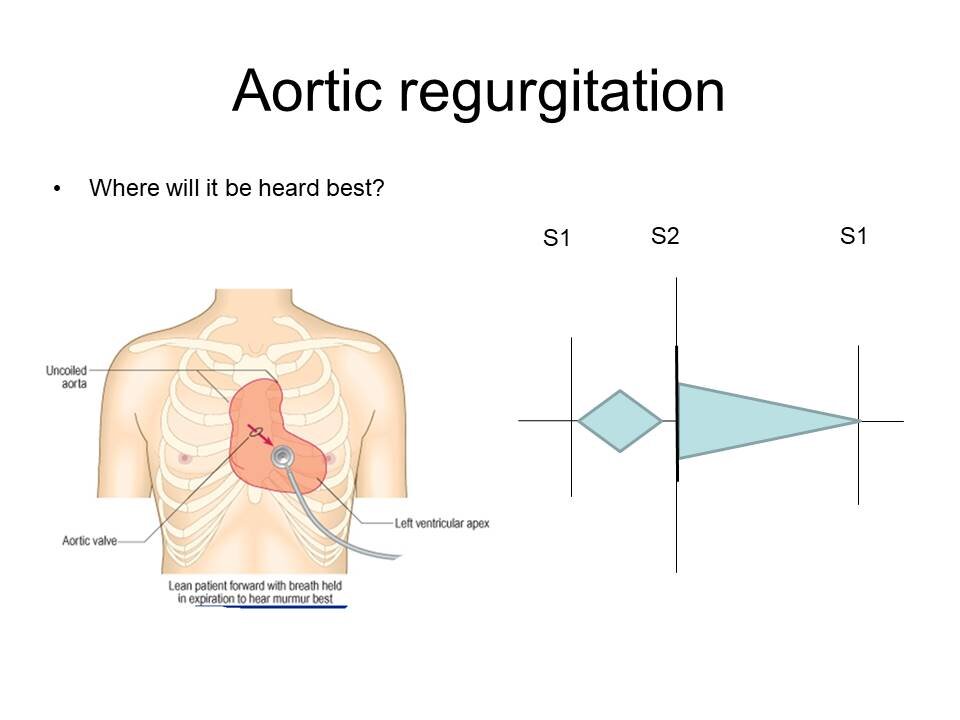
Mitral stenosis and aortic regurgitation are therefore diastolic murmurs.
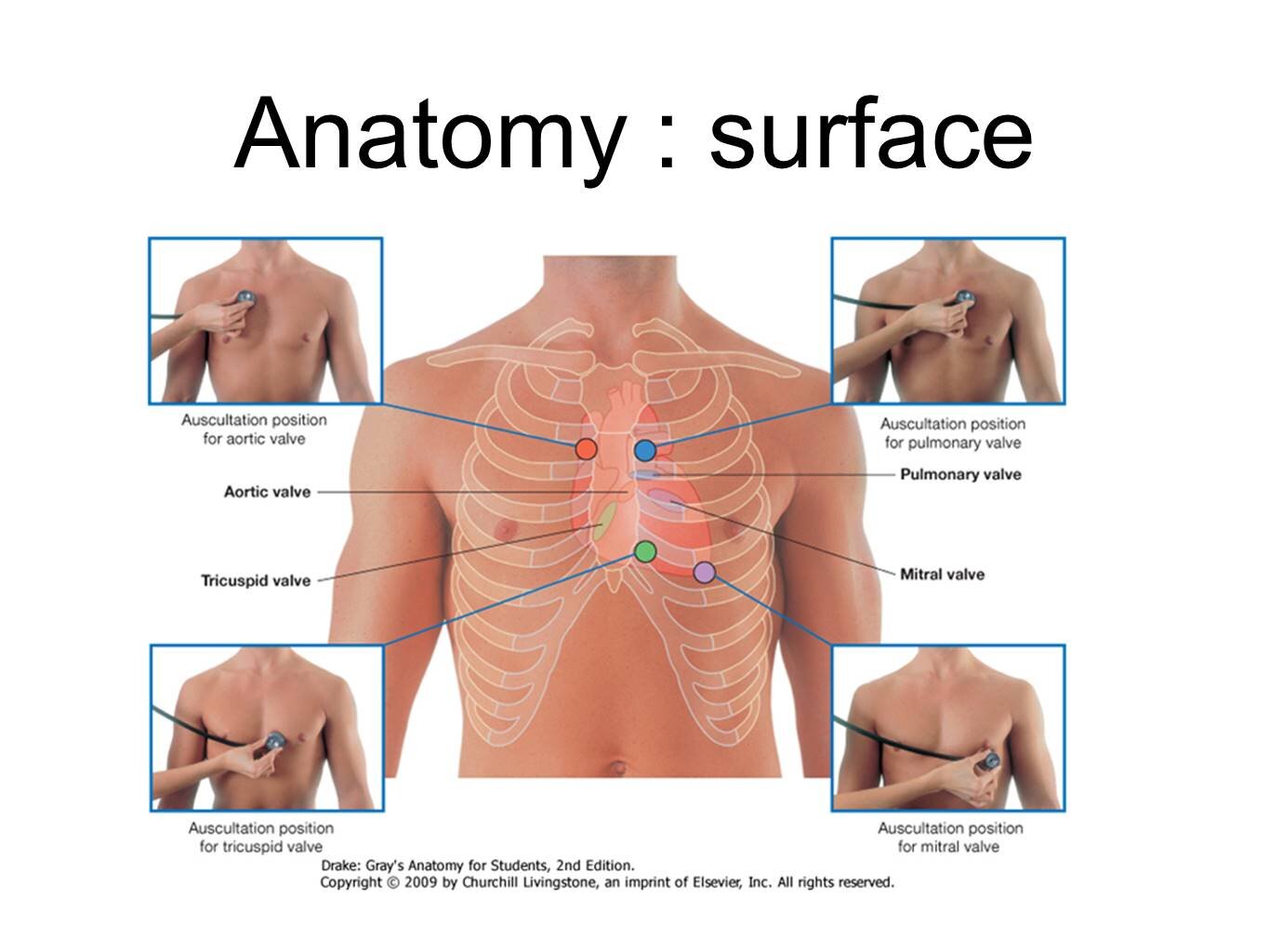
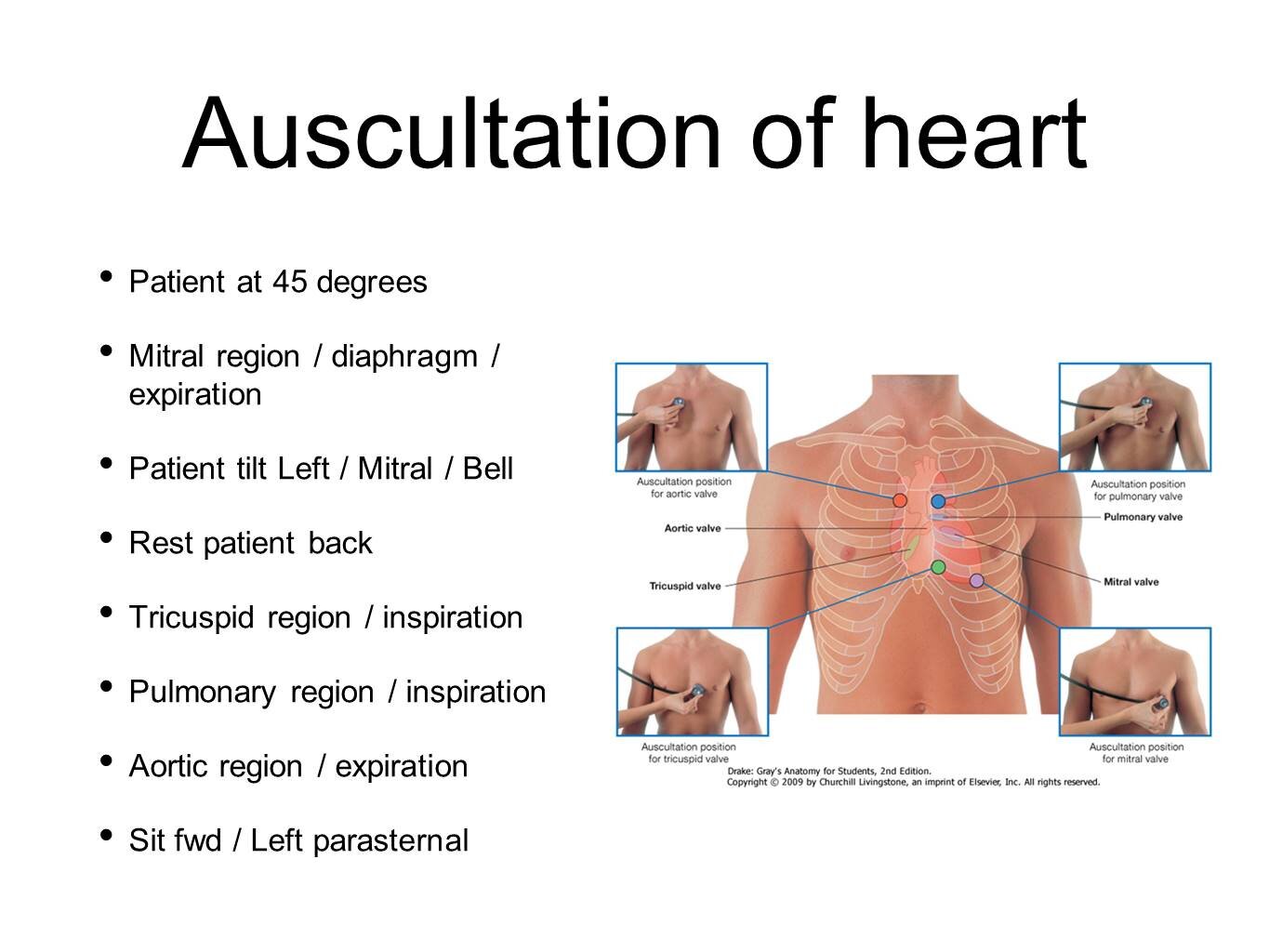
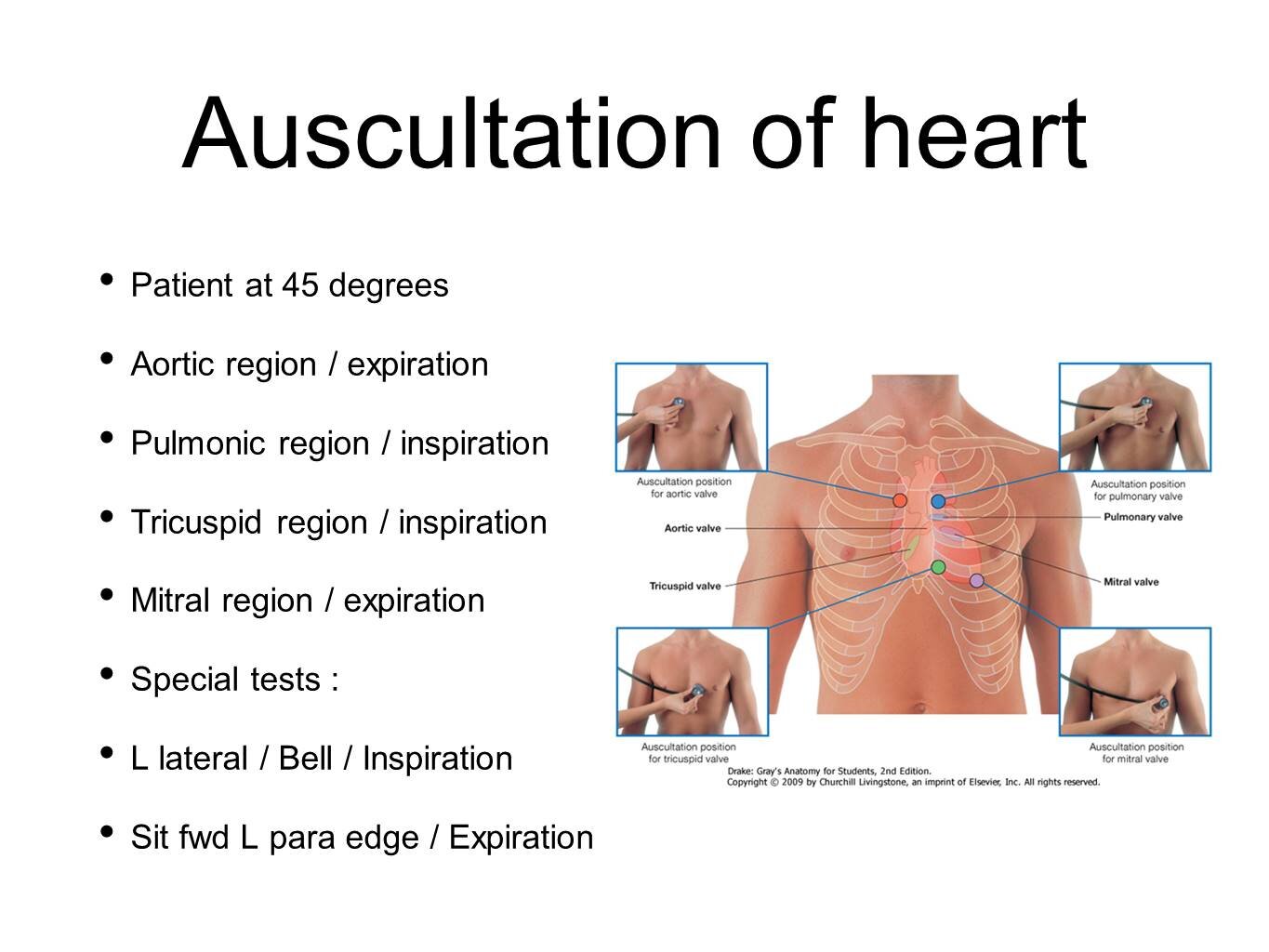
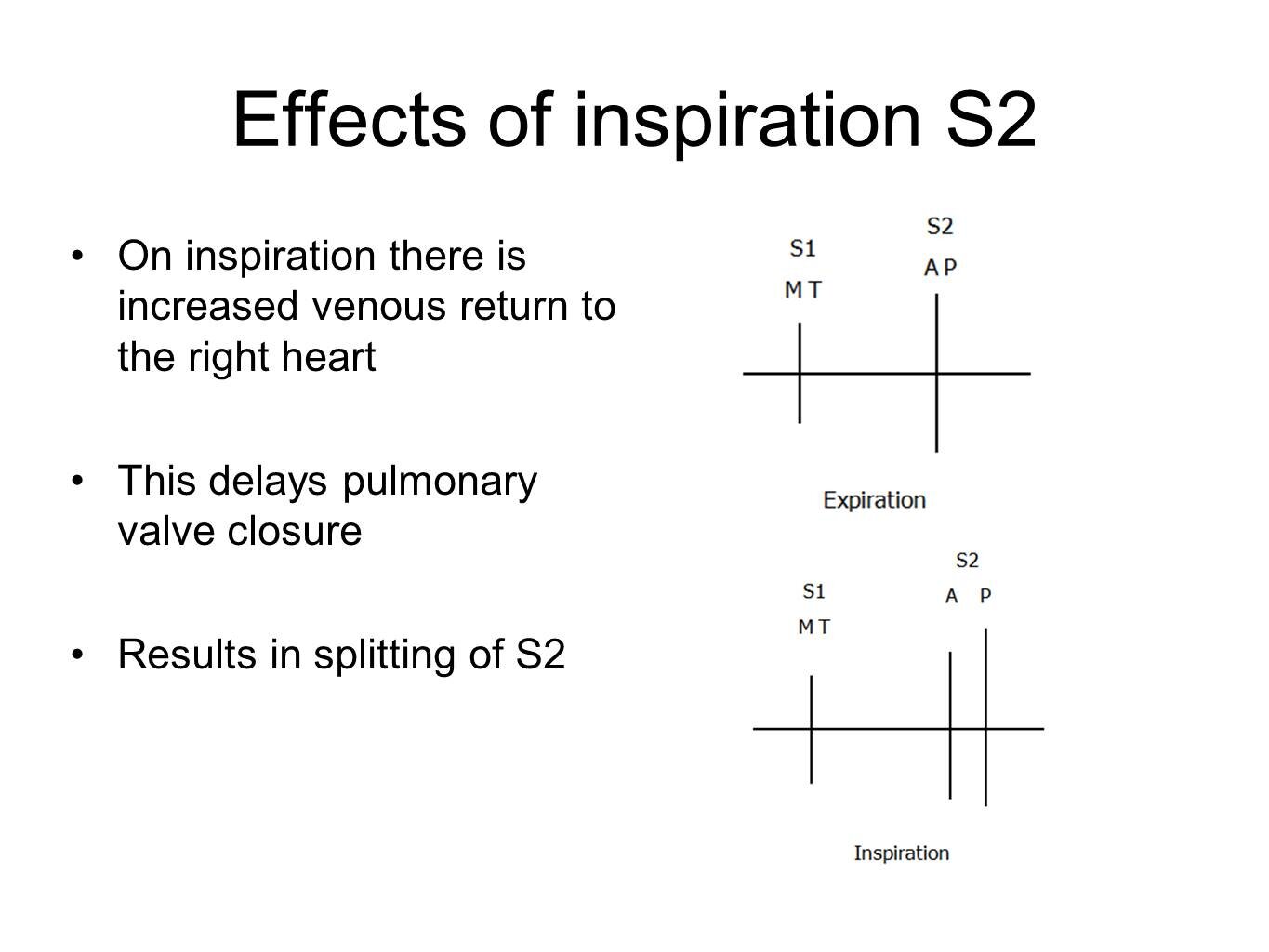
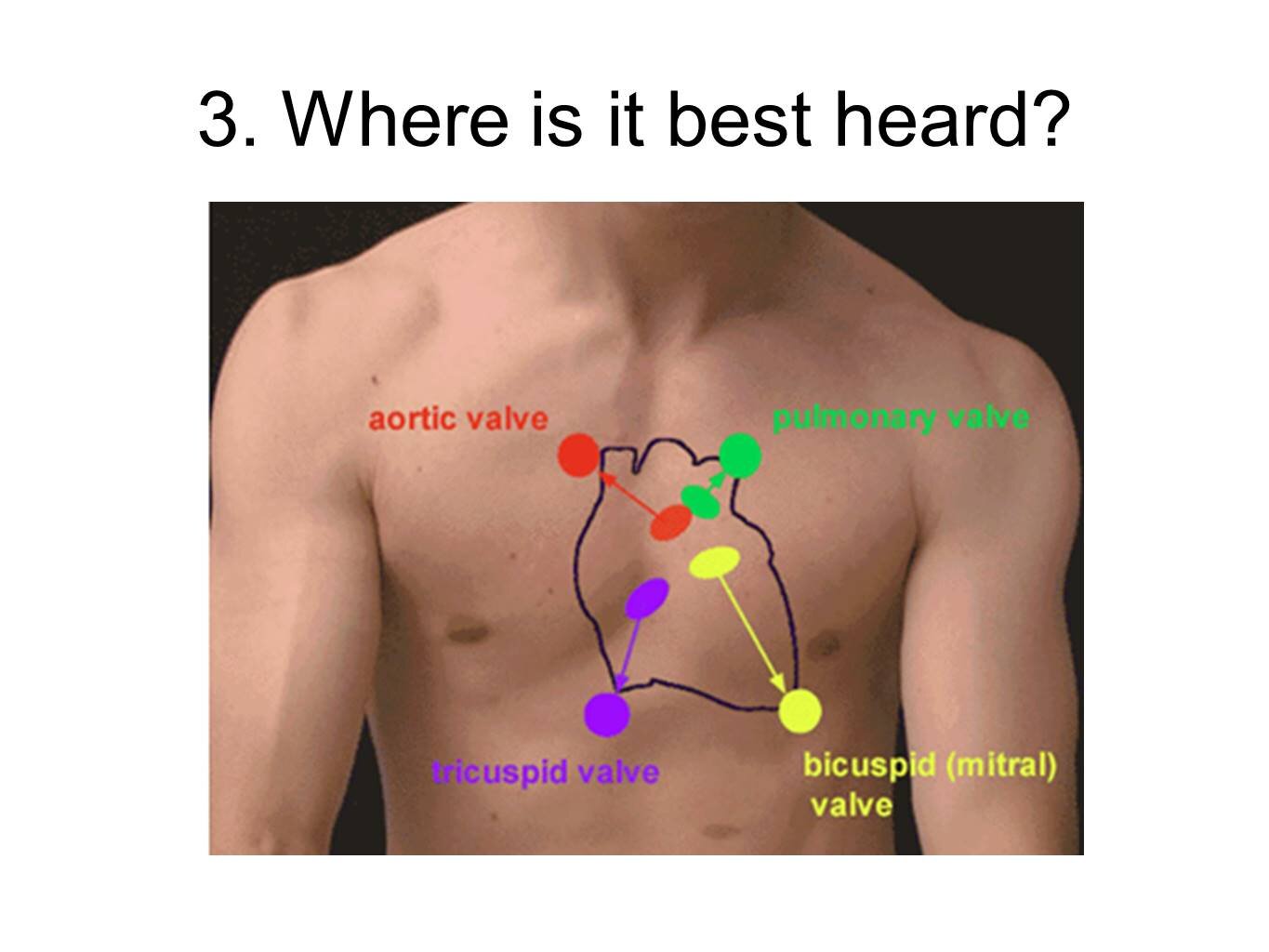
Inspiration reduces intrathoracic pressure and so more blood flows into the right side of the heart. Expiration increases intrathoracic pressure which causes pulmonary vessels to constrict and so blood is forced into the left side of the heart.
The mitral valve is a right-sided valve and so mitral murmurs are loudest during inspiration
The aortic valve is a left-sided valve and so aortic murmurs are loudest during expiration
Here we’ve embedded the aortic and mitral pages from EasyAuscultation.com for you to search:
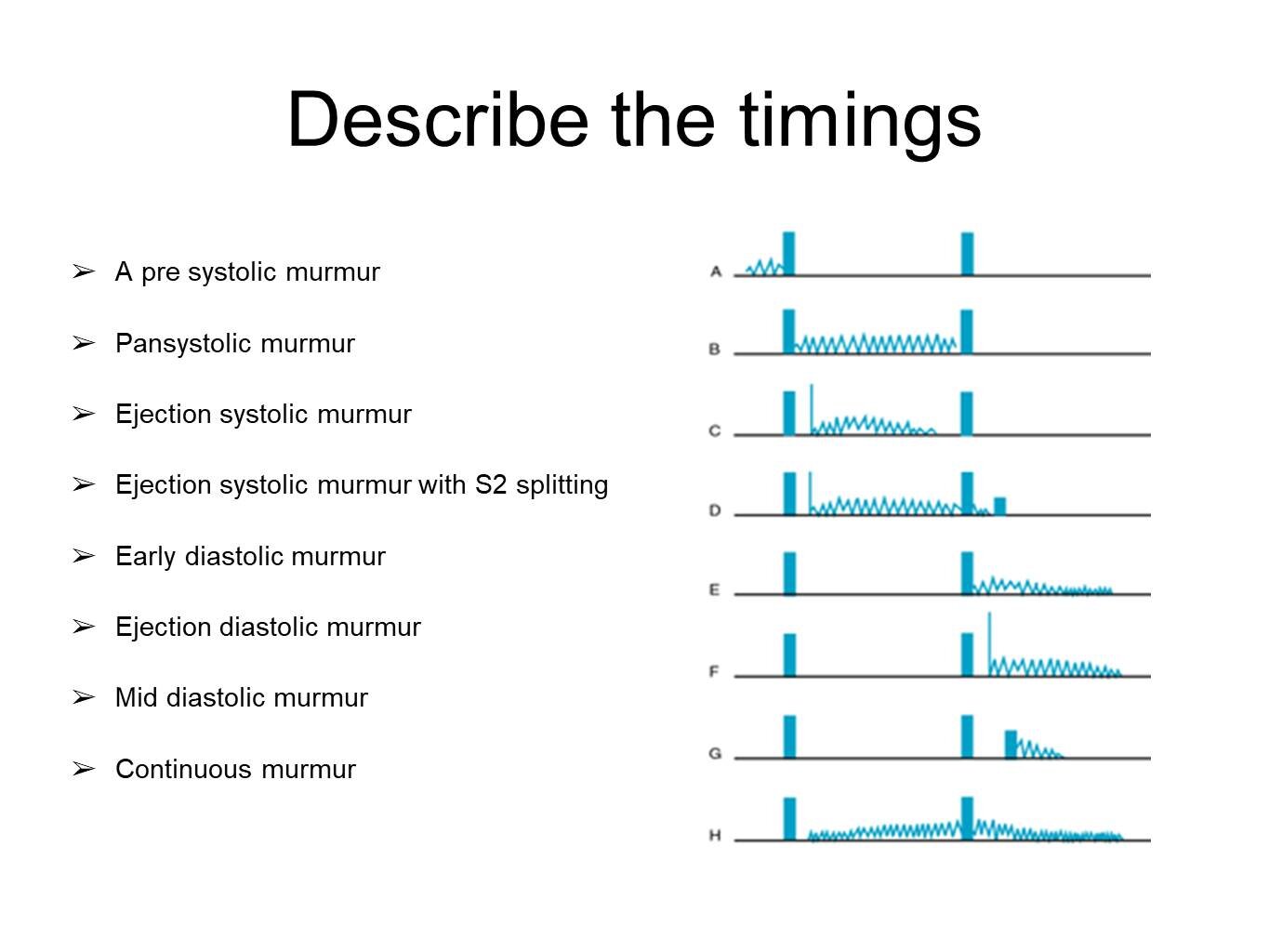
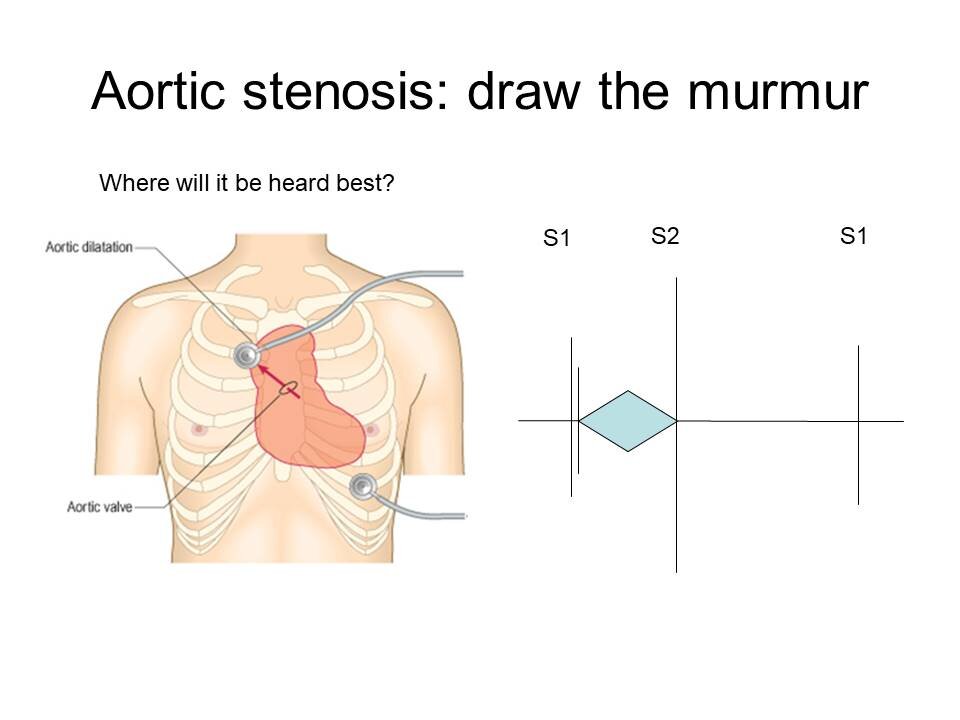
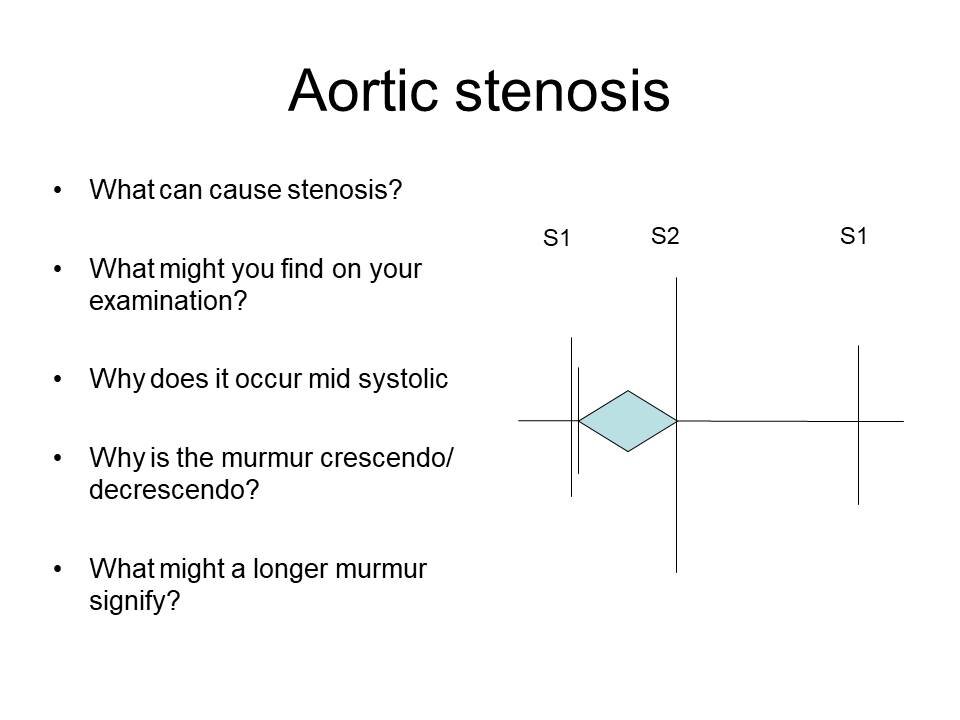
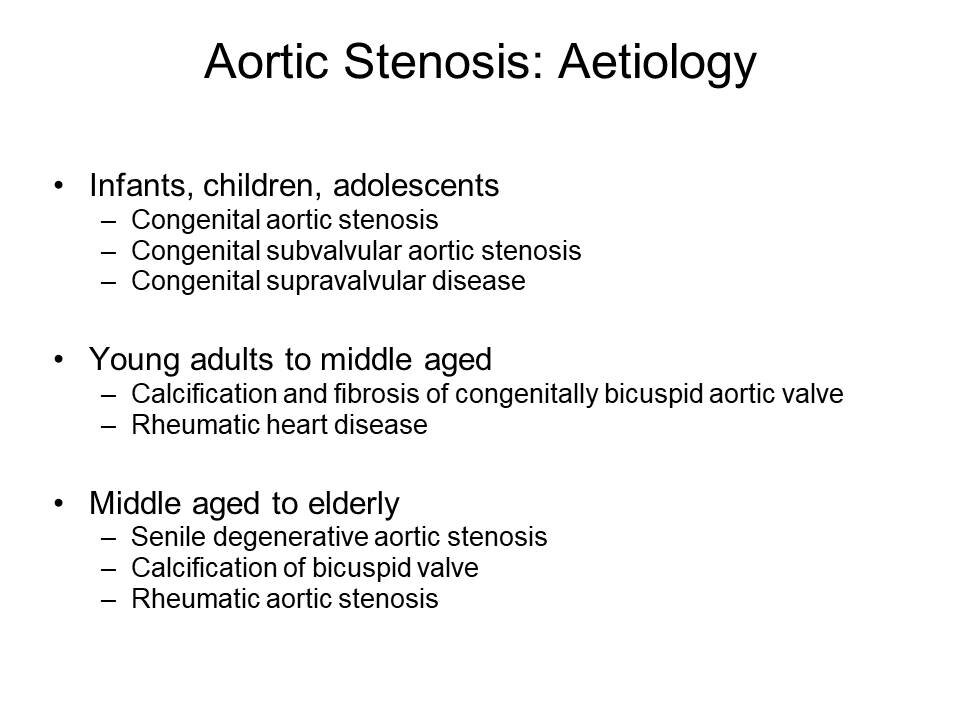
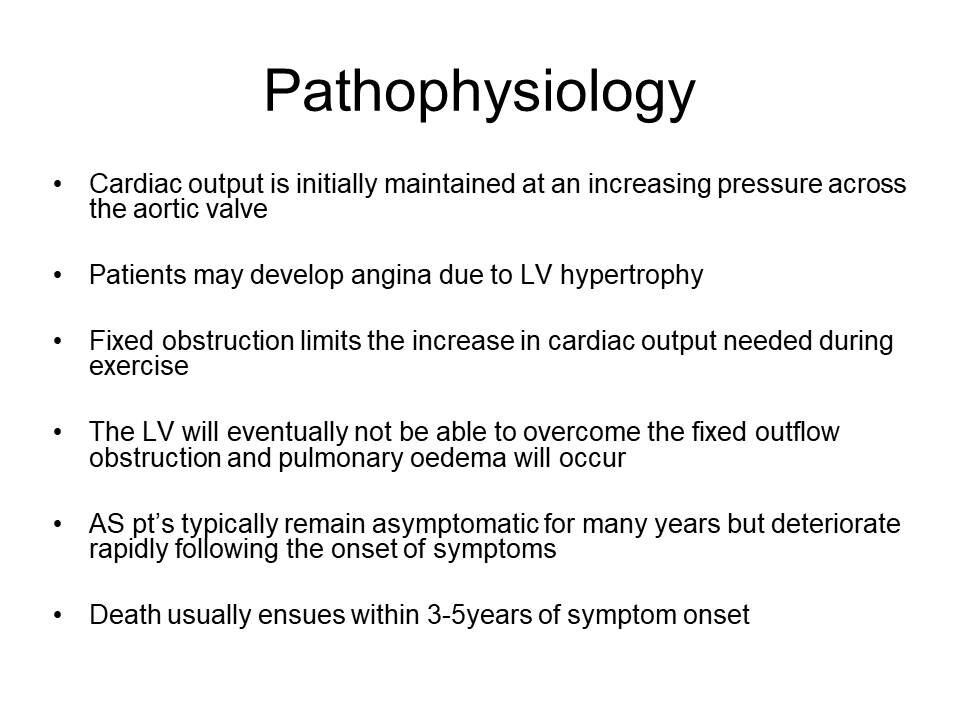
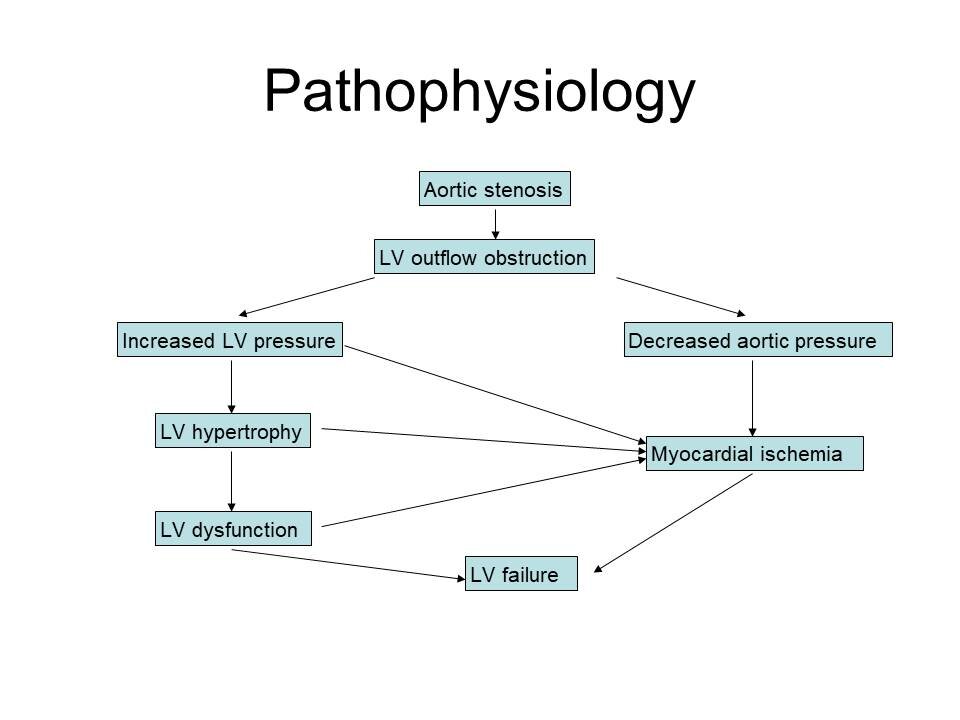
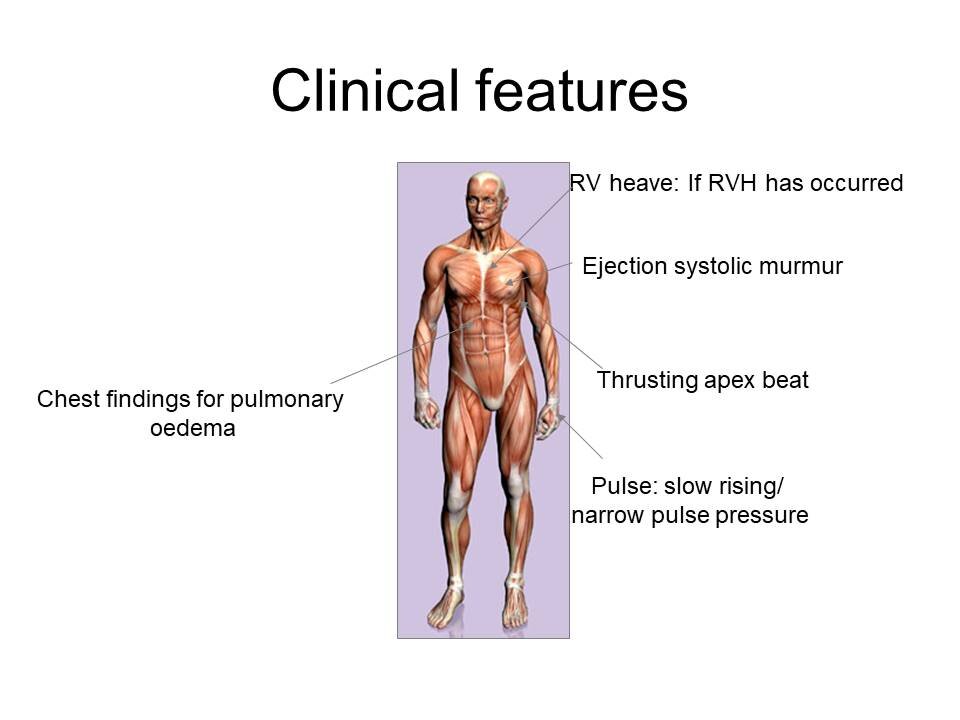
Aortic Stenosis
Ejection systolic murmur
Radiates to carotids
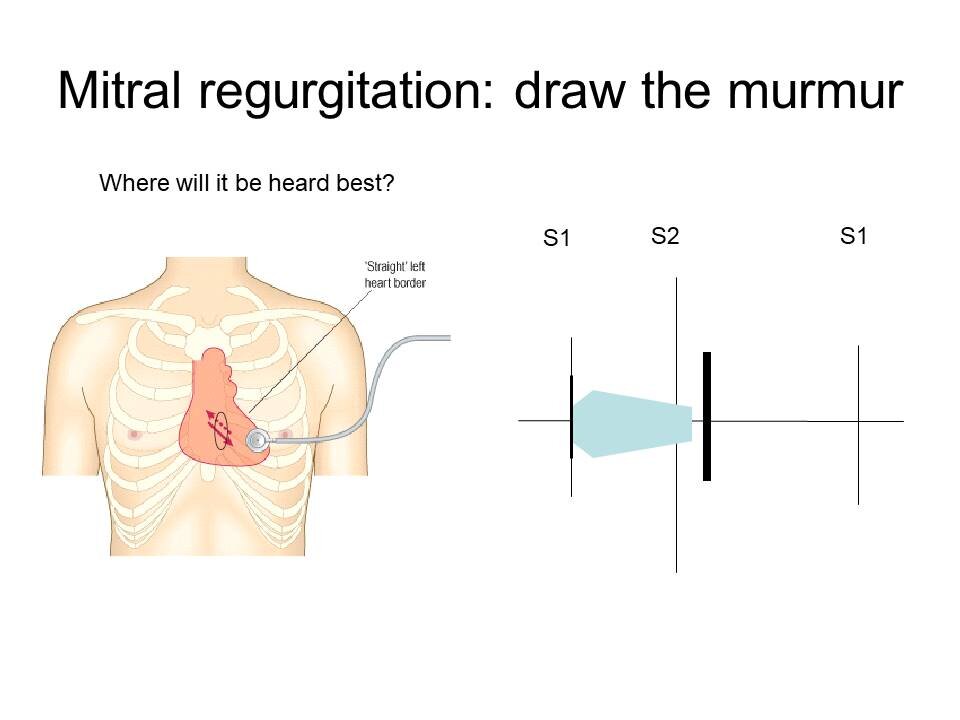
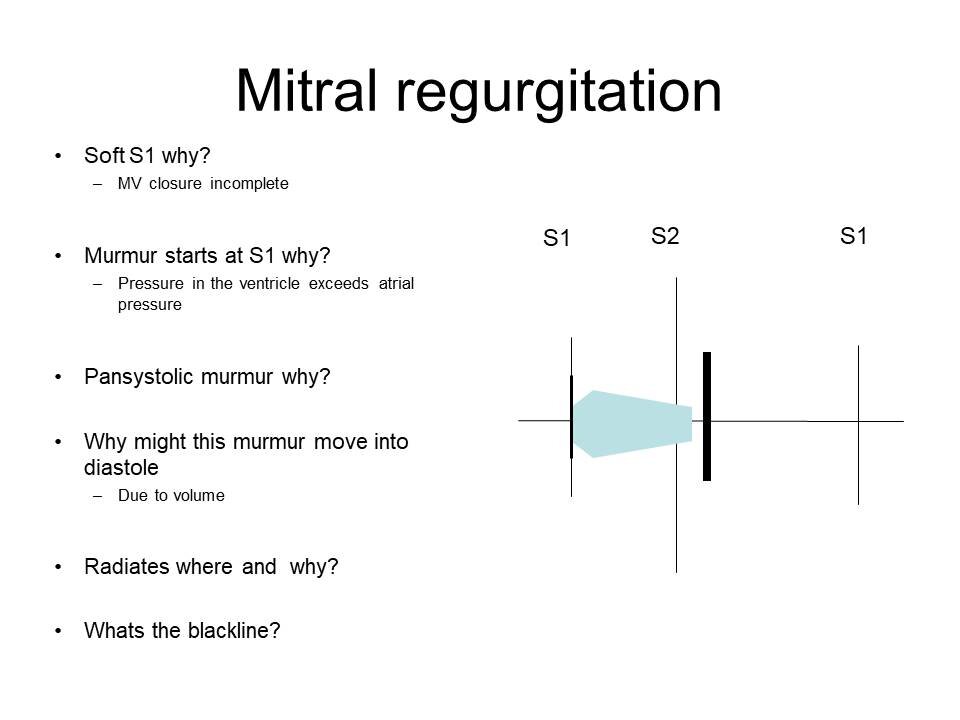
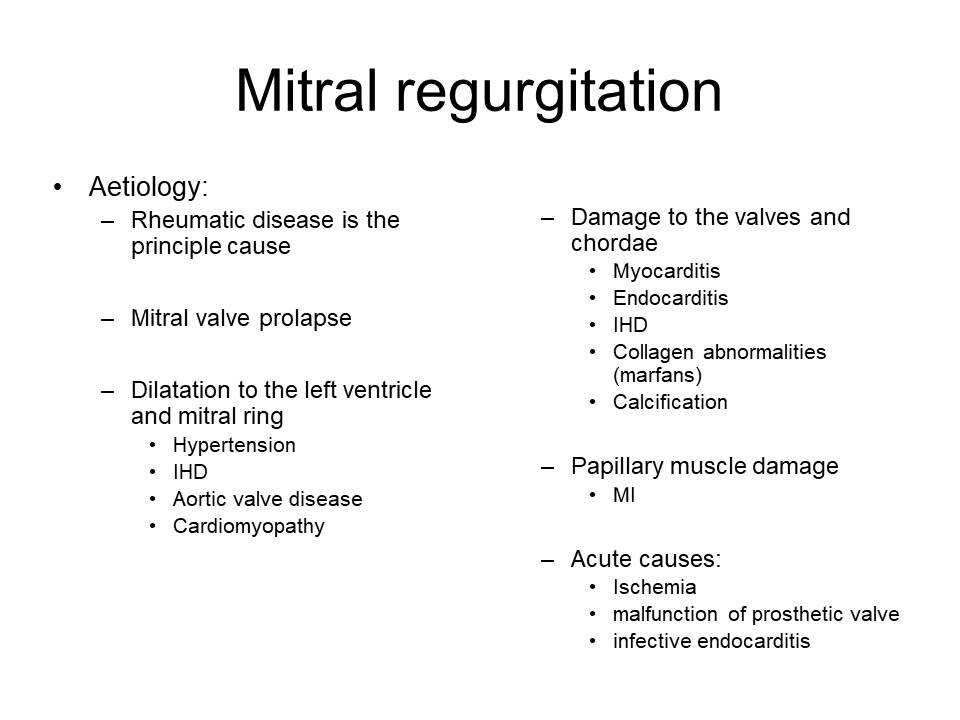
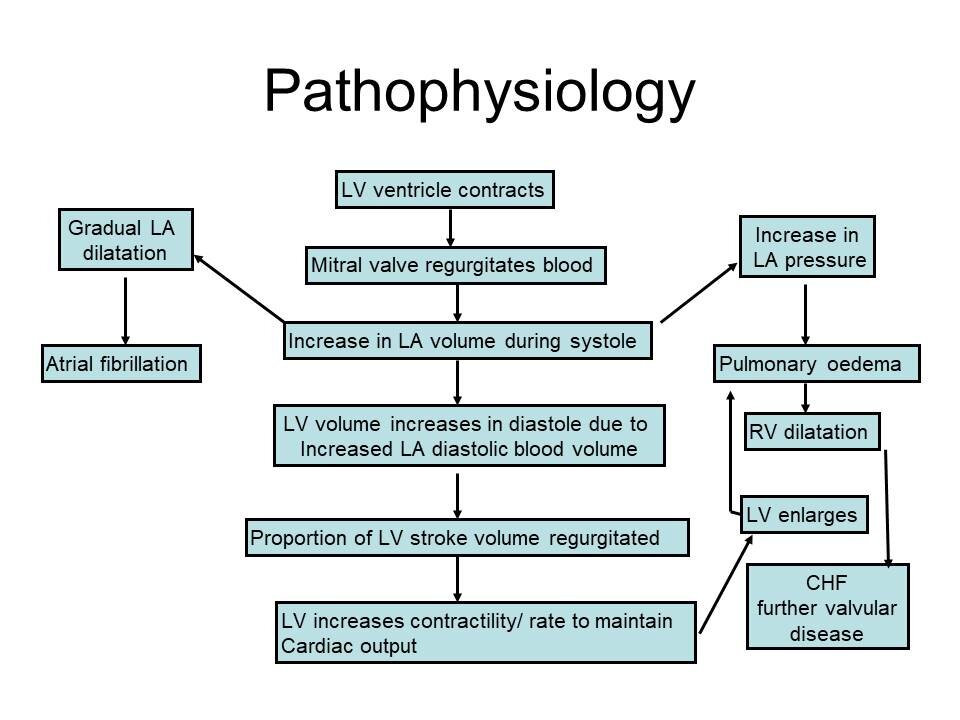
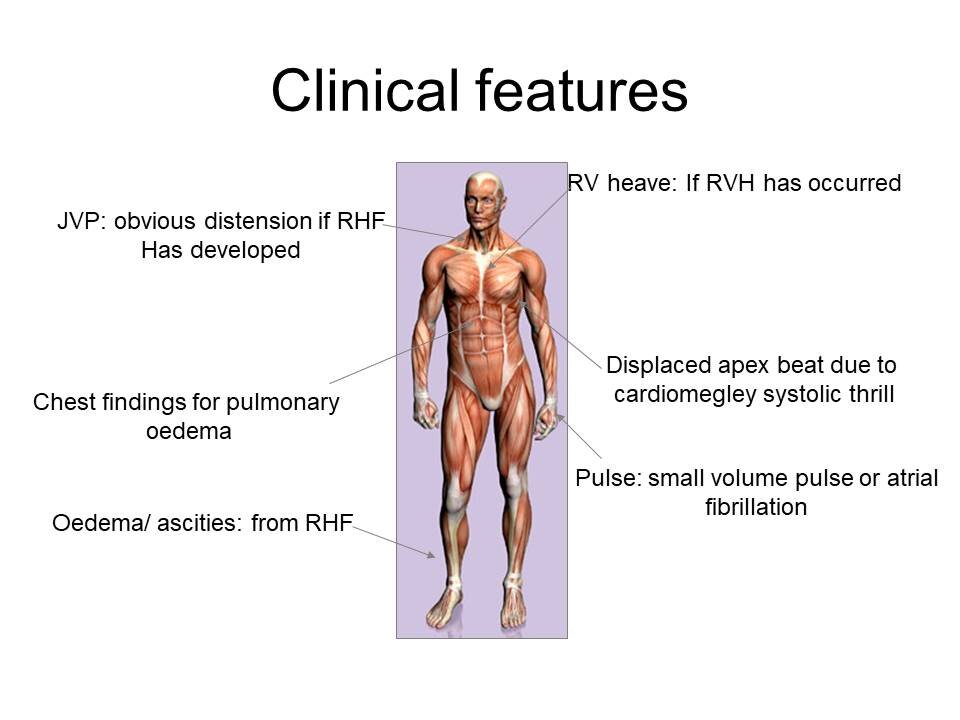
Mitral Regurgitation
Pansystolic murmur
Radiates to axilla
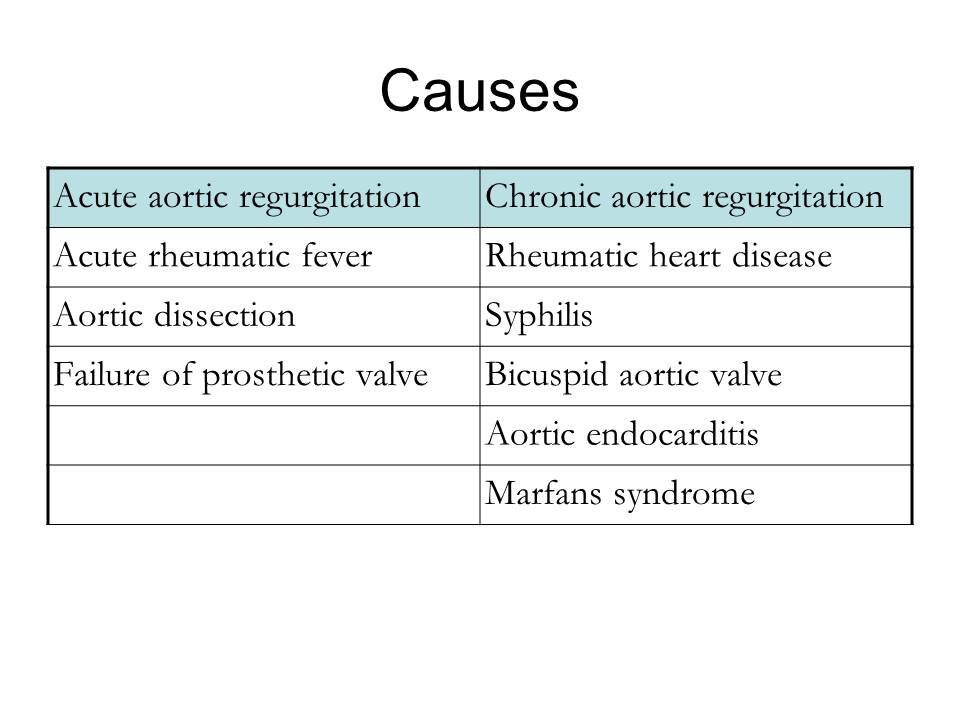
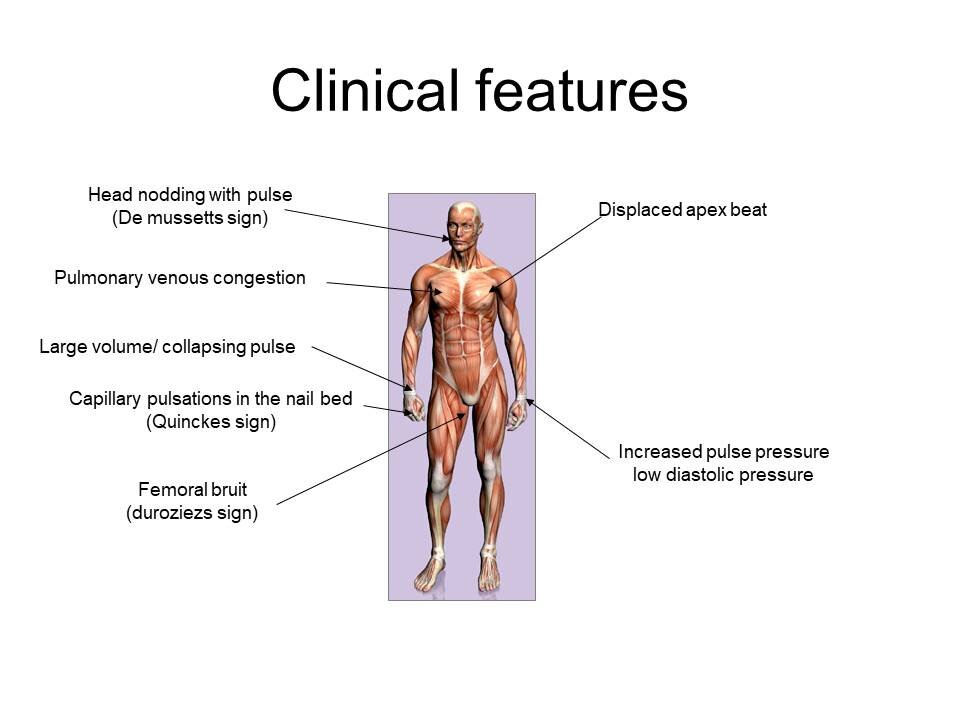
Aortic Regurgitation
Early diastolic murmur
Radiates to apex
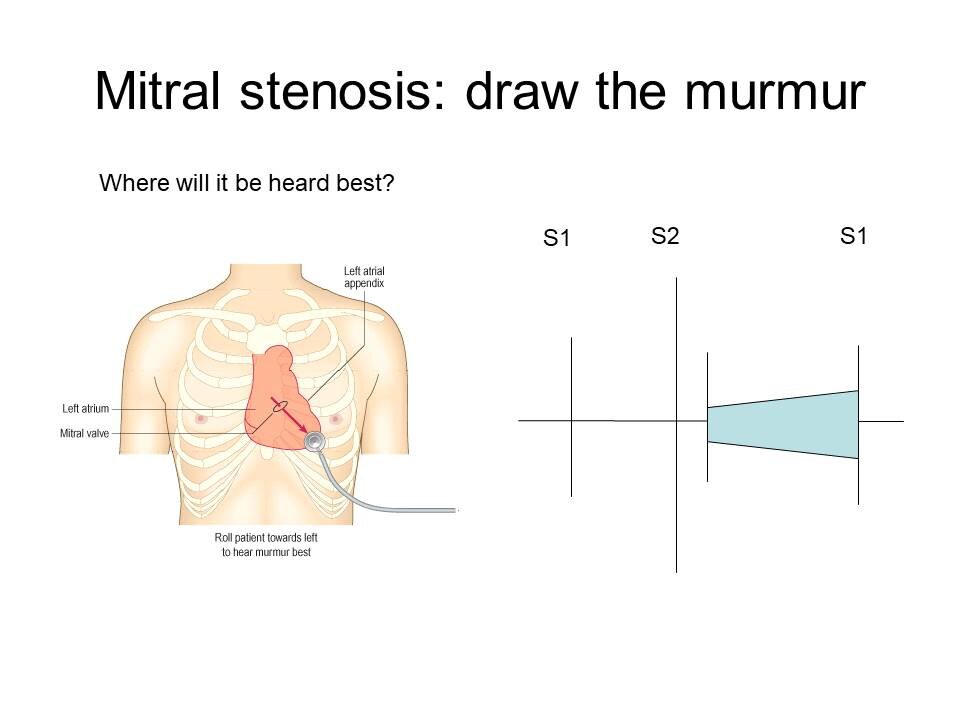
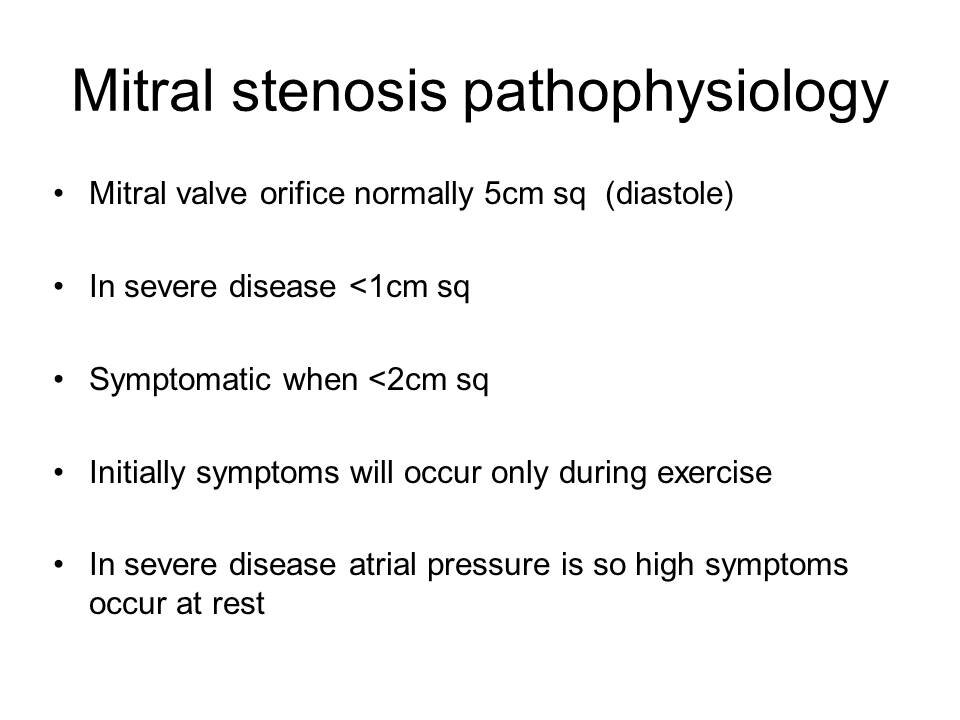
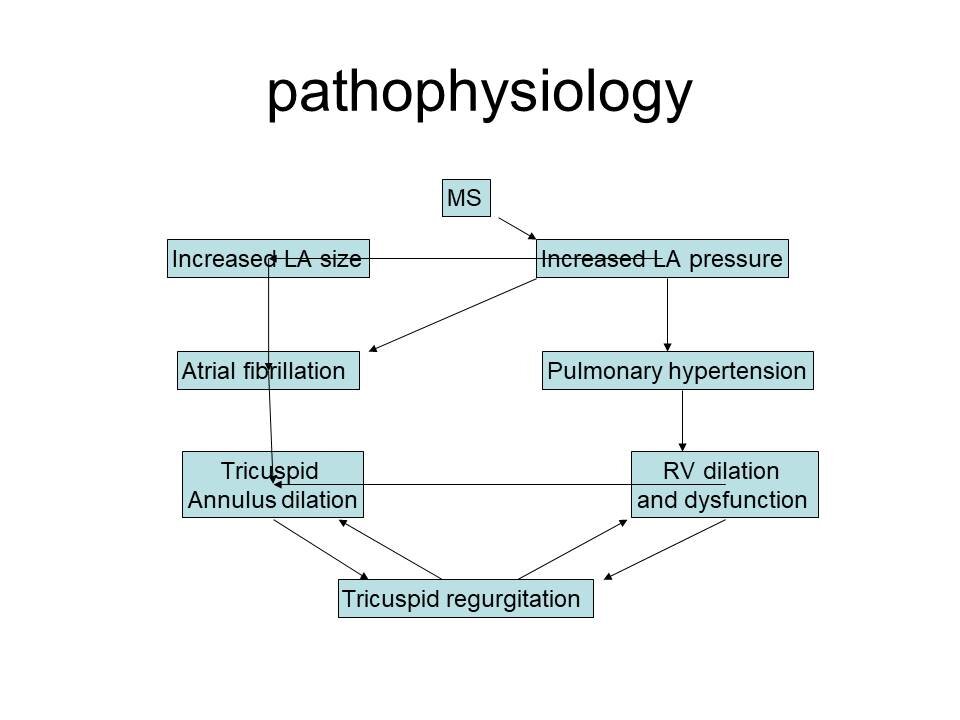
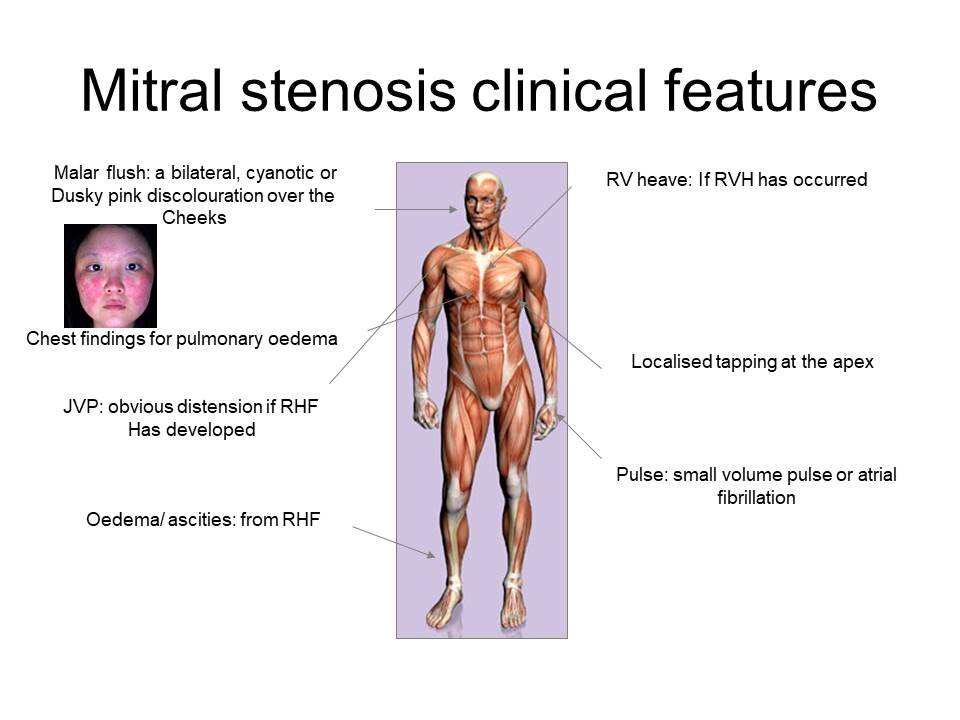
Mitral Stenosis
Clicking sound as valve opens and decrescendo-crescendo diastolic murmur
And here is our #TakeVisually infographic for this episode: