Focused Trauma Conference 2017: Deel Twee
In the second part of the Focused Trauma Conference we were treated to a focus on the role of ultrasound and clam shell thoracostomy.
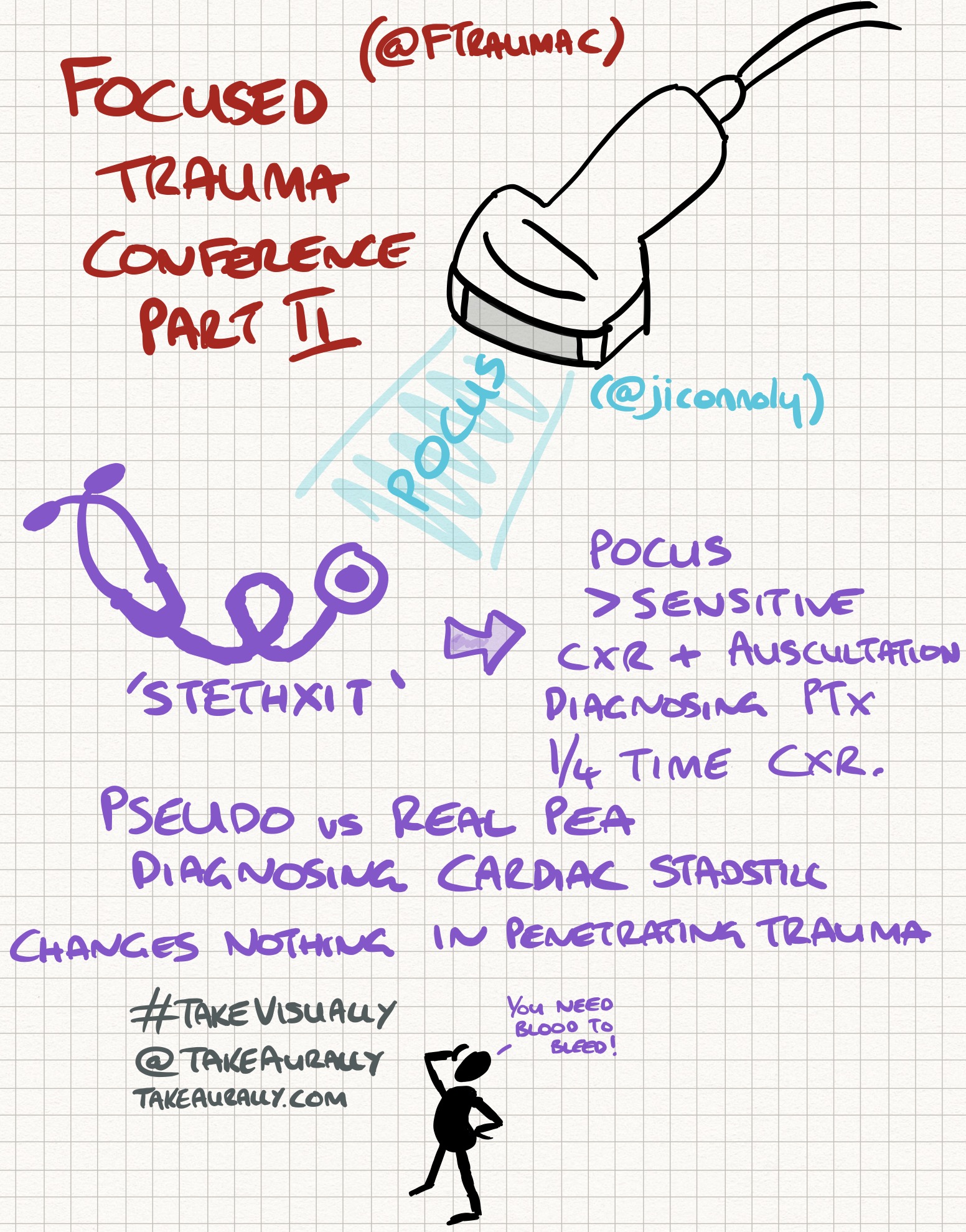
Dr Jim Connolly (@jiconnoly) kicked off the second part by imagining a post-stethoscope world (Stethxit) and instead where we all have hand held ultrasound devices - a reality that's closer than we think - he believes once they crack a cost of <£1000 (i.e. the cost of the new iPhone) a unit we will all have one! POCUS will help identify the majority of causes in cardiac arrest (pretty much all of 4Hs and 4Ts apart from hypothermia or toxins). POCUS reduces the time to operation, the number of CT scans and even the length of stay in hospital. It is time critical, helps with Bayesian reasoning and with answering Yes/No answers. It is more sensitive than auscultation and x-ray in detecting pneumothorax and takes a quarter of the time that CXR does. However it is important to remember its limits:
- A FAST scan needs about 500ml blood in the abdomen to pick up - "you need blood to bleed" and so there may be false negatives
- It changes nothing in penetrating TCA
However in blunt TCA it is useful to pick up cardiac standstill (a very poor prognosis) and also to distinguish pseudo from real PEA.
It was then onto thoracostomy with Professor Lockey and then Dr Connolly again. The procedure was first performed in 1988 and provides better visualisation than the left lateral approach. Professor Lockey talked about the approach in 'street thoracostomy' often performed in cases of stabbings and even terrorism:
- Open the pericardium
- Seal the hole (ideally a single hole in the right ventricle) - occlude with a finger, stitch or staple it or use foley catheter
- Restart the heart - flick it, volume load, 2 handed massage, ventricular adrenaline, given bicarbonate (usually young people getting stabbed so should be fine) and calcium
- Clip the internal mammary arteries and clamp aorta and hilar
- If the patient wakes during anaesthetise with Midazolam 1mg and Ketamine 30mg
- Forensic awareness is also important in cases of stabbings
The whole procedure should take less than 2 minutes. It is not to be performed in cases of shootings/high energy transfer, if the heart is empty or if the TCA has been prolonged.
Dr Connolly reinforced many of these messages as well as emphasising that the biggest barrier to before the clamshell is the fear of being criticised. It is a procedure not an operation designed to achieve damage control and restore physiology NOT anatomy. It is to be performed in witnessed TCA or if there were very recent signs of life or if the systolic BP is <70mmHg despite fluid resuscitation. The wound most likely to survive is a wound to the right ventricle with a tamponade. When suturing a horizontal mattress suture is least likely to occlude the coronaries. He also emphasised the importance of training - at times of stress we revert to our lowest level of training. There are other considerations to have - once output is restored the patient needs to go straight to theatre and can have only vertical sliding not horizontal.
Here are the Take Visually graphics for this podcast: