Suman Biswas at Das SMACC
Not particularly educational but still important to remember to find time for humour! As a fan of the Amateur Transplants it was a real pleasure to see Suman Biswas at Das SMACC and here he is in action. Enjoy!
Not particularly educational but still important to remember to find time for humour! As a fan of the Amateur Transplants it was a real pleasure to see Suman Biswas at Das SMACC and here he is in action. Enjoy!


The other week I watched Jurassic Park being played in Wollaton Park (otherwise known as Bruce Wayne's house). Maybe it's a reflection of how sad I am but I couldn't help but think of Emergency Medicine and FOAMed as I watched this amazing masterpiece of a film. If you haven't watched it now is the chance to stop reading and watch it. You won't be disappointed.
In the scene featuring the Brachiosaurus (see above) the characters are open mouthed and in awe. It's easy to be in awe of Emergency Medicine, especially as you first start, perhaps even intimidated. But there are lessons from this film which can help us as we tackle this majestic speciality.
Embrace education and listen
In the film Lex is nearly eaten by a Tyrannosaurus Rex until Dr Alan Grant tells her to stay still as it won't be able to see her (rubbish but I never said this film was a documentary). She stays still and isn't eaten. Donald Gennaro and Ian Malcolm do move and one is eaten and the other is severely injured. The lesson: listen to your seniors and follow advice especially when faced by a T-Rex or the Triple-A-asaurus.
Educate, don't terrify
In the book by Michael Crichton (who also wrote E.R.) - again read the book if you haven't - Alan Grant loves kids (makes sense as kids love dinosaurs). In the film he hates kids at the beginning before going on a story arc where he loves them. In this early scene he decides to teach a child to respect dinosaurs by terrifying him. The result? One scared child who I'm sure didn't go on to love dinosaurs. We have to inspire as educators not terrify. Those who teach through fear are dinosaurs. Figuratively.
Don't let the little things take you down
The books 'Jurassic Park' and 'Lost World' and the film 'Lost World Jurassic Park' feature small dinosaurs (Procompsognathus in the books, Compsognathus in the film). Whilst little and innocent looking these dinosaurs work together to kill much larger humans. There's a lesson there that if we ignore the small things (not checking bloods, not doing our at work assessments) they can get together and take us down. Don't let them.
Just because you could doesn't mean you should
An important ethics lesson here for all doctors and researchers regardless of speciality. ''First do no harm'.'
Keep it simple...
In the film 'Jurassic World' Ingen decide that as the public are now bored of dinosaurs (as if) to make a new dinosaur the Indominus Rex by mixing the DNA of a T-Rex, Velociraptor, tree frog and, oddly, cuttlefish. The result is a terrifying problem of their own making with multiple traits including, strangely in a creature designed for public display, the ability to camouflage. It's easy in Emergency Medicine to create problems either in our decision making, attitude, human factors...the list goes on. Keep it simple.
...and get help
The Indominus Rex is ultimately only taken down by a tag team effort between Rexy and Blue the Velociraptor with the Mosasaur providing the coup de grâce. Make sure you work as a team. Work on your team work skills. We can then tackle even the biggest problem.
Importance of CPR
A vital skill we all should learn and encourage. No, his technique is not great but at least Dr Grant gives it a try and Tim lives. And it's still better than James Bond's effort in Casino Royale...
Life er finds a way
This classic line from Dr Ian Malcolm sums up everything really. But in the Emergency Department we have to accept there are some things out of our control. There will always be more patients to see. We can't save everyone. We see people at their worst everyday in an environment that shocks people who are new to it. Whilst we should always seek to improve we should also appreciate the sheer amazing job we already do. And accept that sometimes there are somethings we can't change.
There we have it. Lessons from Jurassic Park for the Emergency Department. I'm off to watch Jurassic Park again. Hopefully if we follow these lessons we too can make it on the helicopter home...


Photo by dkidpix/iStock / Getty Images
Just as with ECGs arterial blood gases (ABGs) are an essential part of Medicine and unavoidable. They're a vital part of assessing the unwell patient.
Unfortunately students are often quite blood gas-phobic and this needs to be overcome and hopefully with a stepwise approach we can all learn to love the blood gas! Once again I'll be enlisting the help of Albert Einstein and his chalkboard - the meme generator can be found here.
It's worth saying that ABGs are not nice to receive and so think if you really need to do one or if you could get away with a venous blood gas (VBG). A VBG will give you a reliable pH, bicarbonate, electrolytes, glucose and lactate as well as carbon dioxide if it's normal. ABGs are really good for determining the oxygen partial pressure however. Life in the Fast Lane has a brilliant blog on the subject of VBG vs ABG. This blog will mostly focus on ABGs.
So as ever make sure the gas in your hand is from the right person at the right day and time and look at how much oxygen the patient is on. This is the amount of inspired oxygen or fraction of inspired oxygen (FiO2) the patient is receiving. The delivery device being used by the patient will tell us their FiO2.
Room air at sea level has a FiO2 of 21%.

Photo by Liuhsihsiang/iStock / Getty Images
The next oxygen delivery is nasal cannulae which are only good at delivering 1-4L/m of oxygen - beyond that the patient won't have any benefit and have very turbulent air up their nose! The FiO2 of oxygen delivered by nasal cannula is as follows:
1 L/m = 24%
2 L/m = 28%
3 L/m = 32%
4 L/m = 36%
The next oxygen delivery system to look at are Venturi masks; these deliver a guaranteed FiO2 of oxygen and are brilliant at titrating oxygen to patients especially patients with COPD.

Photo by porpeller/iStock / Getty Images
The Venturi come in different colours and will have the FiO2 written on their side as well as the l/min that are needed to provide that FiO2. Make sure they have the correct flow rate or they won't work. The range available will vary site to site but in the department I work at the Venturi available are 24%, 28% & 40%.
The next highest oxygen delivery system you'll commonly see are non-rebreather masks (NRM).

Photo by Image Source/Stockbyte / Getty Images
"15 litres through a non-breather mask" is a very common statement in an acute A-E station. It's less easy to predict the FiO2 here only that is is somewhere between 60-100%.
Make sure the FiO2 or oxygen delivery is documented on the gas.
pH: 7.35 – 7.45 (pH messages the amount of Hydrogen ions in a solution (in this case blood) the lower the pH the more acidic the blood, the higher it is the more alkalotic it is)
There are two main components contributing to the pH - the respiratory side (CO2) and metabolic (Bicarbonate). A problem with one can be compensated with the other - more of that later.
PaCO2: 4.7-6.0 kPa (Pa stands for Partial Pressure - the amount of pressure the gas in question contributes to the atmosphere measured in kilo Pascals. CO2 is acidic when dissolved in solution. Increasing respiration rate blows off CO2 while reducing respiration rate means we retain CO2. Normally PaCO2 is what drives our ventilation; this is not the case in chronic CO2 retention such as COPD where hypoxia then drives respiration)
PaO2: 11-13 kPa (if this is low then the patient is hypoxia - this is cause of cardiac arrest and so must be identified early)
HCO3-: 22-26 mEg/L (Bicarbonate is basic and so is used as a buffer against acid. Increasing the amount of bicarbonate however takes hours to days whereas it's almost instantaneous to alter respiration rate)
Base excess: -2 to +2 mmol/L (this is measure of the metabolic component of a problem with the pH. If the BE is below -2 then the patient has a base deficit and so has metabolic acidosis. If the BE is above +2 then the patient has a base excess and a metabolic alkalosis

Once you're happy with the ABG being for the right patient etc it's now time to first look at the pH - is it normal, high (alkalotic) or low (acidotic)?
Is the CO2 normal, high (hypercapnic) or low (hypocapnic)?
Is the O2 normal, high (hyperoxic) or low (hypoxic)?
At this point we need to remember the Alveolar-arterial (A-a) gradient. This is the gradient between the PaO2 of inspired air and that in the blood. In a healthy adult it should be about 5-10mmHg. That means the PaO2 on your ABG should be about ten less the FiO2, hence why in room air (FiO2 21%) the normal range of PaO2 is 11 - 13 kPa.
A-a gradient is accurate up until FiO2 of about 60% and over. Why is it important? Well, you could have a patient on a 28% Venturi with normal saturations but if their PaO2 is less than 18 kPa (say 12 kPa) then they have relative hypoxia and we should be more worried about them and make sure they are getting senior support.
If the patient is hypoxic check the PaCO2 again
If PaO2 is low and PaCO2 is low or normal then the patient has Type 1 Respiratory Failure - the lungs are failing in the function of taking O2 from the air to blood

If the PaO2 is low and PaCO2 is high then the patient has Type 2 Respiratory Failure - the lungs are failing in getting O2 from the air and removing CO2 from the blood. This may be acute, chronic or acute on chronic. The raised PaCO2 will lower pH acutely; the blood will respond by buffering this by increasing bicarbonate production in the kidneys. This process takes days to hours. Patients may walk around with a fully compensated Type 2 Respiratory Failure (such as COPD) but then decompensate and become acidotic again despite the raised bicarbonate - acute on chronic failure
Acute Type 2 Respiratory Failure (no compensation):
pH 7.2
PaCO2 10
Pa O2 7
Bicarbonate 24
Chronic Type 2 Respiratory Failure (fully compensated):
pH 7.39
PaCO2 10
PaO2 7
Bicarbonate 30
Decompensated Chronic Type 2 Respiratory Failure (Acute on Chronic):
pH 7.28
PaCO2 11
PaO2 6.8
Bicarbonate 30
Causes of Type 2 Respiratory Failure can be pulmonary (such as COPD); peripheral (such chest wall deformities or peripheral nervous diseases such as Motor Neuron Disease) or central (such as overdose of opiates or benzodiazepines causing respiratory depression)
So now we know the values for pH, PaCO2, PaO2 and Bicarbonate it's now time to put it together and identify whether it is a Respiratory or Metabolic cause for pH disturbance
I use the mnemonic 'ROME'
The problem is Respiratory when the PaCO2 is Opposite to pH
The problem is Metabolic when the bicarbonate (HCO3-) is Equal to pH
I find this is a very quick way of identifying the cause, being aware of course that you can have mixed acidosis (due to combined high PaCO2 and low bicarbonate) and mixed alkalosis (low PaCO2 and high bicarbonate)
If the problem is respiratory then there will be metabolic compensation (compensating high PaCO2 with high bicarbonate and vice versa) - this takes a long time remember
If the problem is metabolic then there be respiratory compensation which is much quicker
Compensation can be none, partial (there is an attempt but pH remains deranged) or full (pH back within normal limits)
Remember that there are other bits of information on an ABG
Sodium
Potassium - if deranged do not wait for serum U&Es before commencing treatment
Calcium
Chloride
Glucose - while BM machines will just say 'HI' once BM ~30 the ABG will measure up to about 50
Lactate - important measure of tissue perfusion
Haemoglobin - not entirely accurate but will give an idea of anaemia/bleeding
Carboxyhaemoglobin
It is important not to miss this information as well!
There is a brilliant RCEM module on ABGs here.
Check out the brilliant Geeky Medics page on ABG interpretation here.
It's that time of year again; the medical new year where 5 years of medical school comes to fruition and students become F1 doctors. I've thought back to my time as an F1 and here's 50 tips. If you don't get the Sunscreen reference then I'm officially old...
39. It's not OK to not be OK. Talk to someone. 40. There is nothing more contagious in healthcare than emotions. Smile. Be positive and it will spread. 41. Doctors consistently are amongst the most respected professions. Never abuse that trust. 42. Remember #HelloMyNameIs. 43. Always get your sleep. 44. Coffee is your friend. 45. You should always get more out of alcohol then it gets out of you. If that changes get help. 46. Pain and Urinary retention are two important causes of agitation.
47. Be careful what you post on social media.
48. Not matter how hard breaking news is for you it is worse for the patient/family receiving it.
49. Chew your food. Especially watermelon - trust me on this.
50. Wear sunscreen.
THIS IS THE ORIGINAL MUSIC VIDEO Great Music video from the nineties ! The lyrics are taken from a famous essay - written in 1997 by Mary Schmich, a columnist with the Chicago Tribune - which gives some amazing advice for life, thoroughly recommend everyone to watch this ! enjoy !
ECGs are an essential part of Medicine and unavoidable as a student and junior doctor. I remember being bleeped as an F2 on call by an Orthopaedic surgeon to read the ECG of one of his patients as he had forgotten...ECGs are definitely a case of improving confidence and knowledge through repeated practice and exposure.
Once again I cannot recommend Life in the Fast Lane enough for incredible resources when it comes to ECG.
Here is our video on how to take an ECG:
In the latest Take Aurally podcast I discuss an approach to ECG interpretation and in this blog I've enlisted the help of Albert Einstein to help me through. You can find the tool for making this meme here.
Remember, it doesn't matter how the patient describes their chest pain as an ''ache'', ''twinge'', 'indigestion''...whatever chest pain is chest pain and needs an ECG.
This step is vital, is the ECG in your hands from the right patient, right day and time? Also, get an idea about the presentation behind the ECG, do they have pain, shortness of breath, collapse or palpitations?
Only in certain BBC television dramas (cough, Casualty, cough) does a flat line on an ECG mean death. In real life it means that the ECG lead in question is not connected properly and needs reattaching. Make sure you can see electrical activity in all 12 leads.
Most ECGs will tell you this anyway but it is important to be able to work this out for yourself. In a regular rhythm (equal distance between all R waves) you can count the number of large squares between each R wave and divide 300 by this number. Alternatively you can count the number of beats on the rhythm strip and times this by 6.
There's about 3.5 big squares between each R wave here. Using 300/3.5 gives a heart rate of 86.
Alternatively, there are 15 beats on the rhythm strip, 15 x 6 = 90.
This is all about looking at the R-R distance for successive beats. This can be marked on a separate piece of paper and moved along to confirm.
If the rhythm is irregular you can then also see if it's regularly irregular or irregularly irregular
By looking at successive R-R distances we can see that this ECG shows a regular rhythm.
The QRS complex should be 3 small squares wide. This is important for two reasons. In tachycardia the duration of QRS points to the diagnosis and management as shown in the Resus Council flowchart below. In normal rates it also points to a bundle branch block.

Taken from Resus Council UK
My method for working out LBBB or RBBB...without a William or Marrow in sight
P waves indicate sinus rhythm. PR interval should be 3-5 small squares.
First degree heart block: PR interval is prolonged and remains the same (occurs between SA and AV node)
Second degree heart block: Mobitz 1 - the PR interval gets longer and longer until there is a dropped QRS and the cycle starts again. (Occurs in the AV node) Mobtiz 2 - the PR interval is long, stays the same length but there is a dropped QRS in a ratio: 3-1, 4-1 etc (occurs after AV node in bundle of His/Purkinje fibres)
Third (complete) heart block: No relationship between P waves and QRS (occurs anywhere from AV node down)
PR interval could also be shortened as seen in WPW.
Axis is all about the general spread of electrical activity across the heart.
Here I look at leads I and II. Usually the R waves should both be positive as here:
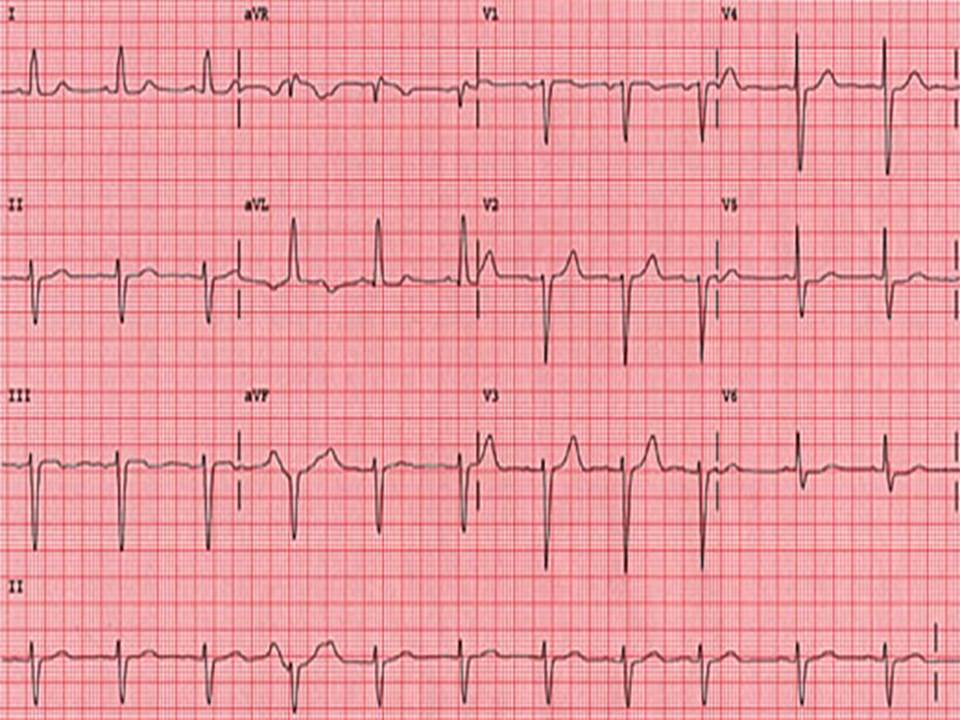
In left axis deviation the R wave in II is now negative so they pointing away from each other or 'leaving'.
Leaving = Left Axis Deviation
This is a sign of ischaemia

Here the R wave is I is negative so they reaching for each other.
Reaching = Right axis deviation
RAD is a sign of RVH

This is important to notice ST elevation - STEMI (2mm or more in 2 or more chest leads or 1mm or more in 2 or more limb leads) or ST depression or T wave inversion - can be seen in NSTEMI
Be wary if you see regional ST depression - this could be reciprocal depression so make sure you look for ST elevation in other leads
Remember to look at the J point - the point where the S wave joins the ST segment - this can be raised in young, thin patients giving the appearance of ST elevation. This is caused benign early repolarisation or 'high take off'
T waves can also point to other conditions - the tall T waves in hyperkalaemia; biphasic T waves in hypokalaemia or ischaemia; or flattened in ischaemia or electrolyte imbalance.
U waves, small deflections after the T wave can be seen in a number of conditions; hypokalaemia, hypothermia or antiarrhythmic therapy like digoxin
It was an honour to be asked to present at the 4th annual Undergraduate Medical Education Conference (UMEC) at the University of Nottingham on 7th July. It's a great opportunity to see the great work being done to improve the teaching of our students.
I think we were all impressed by the work of WAMS (Widening Access to Medical School) a programme run by medical students in association with work by the university to widen access to students who might otherwise not go to medical school. I was very lucky with the support from home I received; many are not so lucky.
The DREEAM team out in force for UMEC 2017.
It was great to hear from my fellow podcaster Charley Peal on her work 'Nifty Fifty' giving clinical students a booklet of 50 challenges such as escorting a patient to X-ray to help them orientate and stay on the ward. Or as she and her fellow medical fellow Becca Noble put it ''avoid being a trip hazard''. Not saying I actually caused people to trip up when I was a medical student but I certainly had some near misses.
There was a good discussion about the difficulties of sharing educational resources. This is why I support FOAMed despite its detractors. No paywall; no firewall. The challenge is quality control of course but I've often thought that there's great work going on that just isn't celebrated enough. I've regularly been in conferences and felt it just seems like some institutions are better than others at getting their message out there. There must be reasons at the individual level to explain this but it must also be due to leadership and the culture of an institution.
We also discussed the conundrum at the heart of medical education I feel. Our students want to pass exams. We want them to be safe doctors. It's sad but understandable when in the past I've had to cancel sessions because they're near exams and whilst they'd help the students as doctors I know engagement would be poor if I put it on.
My DREEAM colleague Matt Govan kindly filmed me. It's actually hard to boil a subject down into 7 minutes and it took a lot of practice. Looking at it I hope it shows a progression with using the P3 approach to presentation. The last time I presented I was told I dance about a bit so here I'm routed to the spot by 'anchoring' against the podium.
In my last blog at Das SMACC I mentioned how SMACC has helped change the approach to conferences at this philosophy was evident at UMEC; short presentations, workshops dotted amongst the schedule with social media being used throughout. As someone who attends a lot of conferences it's a great development and one to be continued. Thanks to everyone at the UMEC organising committee.
And so Das SMACC ist fertig and I am sat in my office in Nottingham reflecting on an amazing three days. Thank you to all who made Das SMACC happen and thank you to my colleagues for accompanying me on the ride, tolerating me and allowing me to convert their voices into MP3 format.

So, Day Three. It's fair to say that I was not in the best of humours at the beginning of the day which may have had something to do with the Das SMACC party the night before. Maybe.
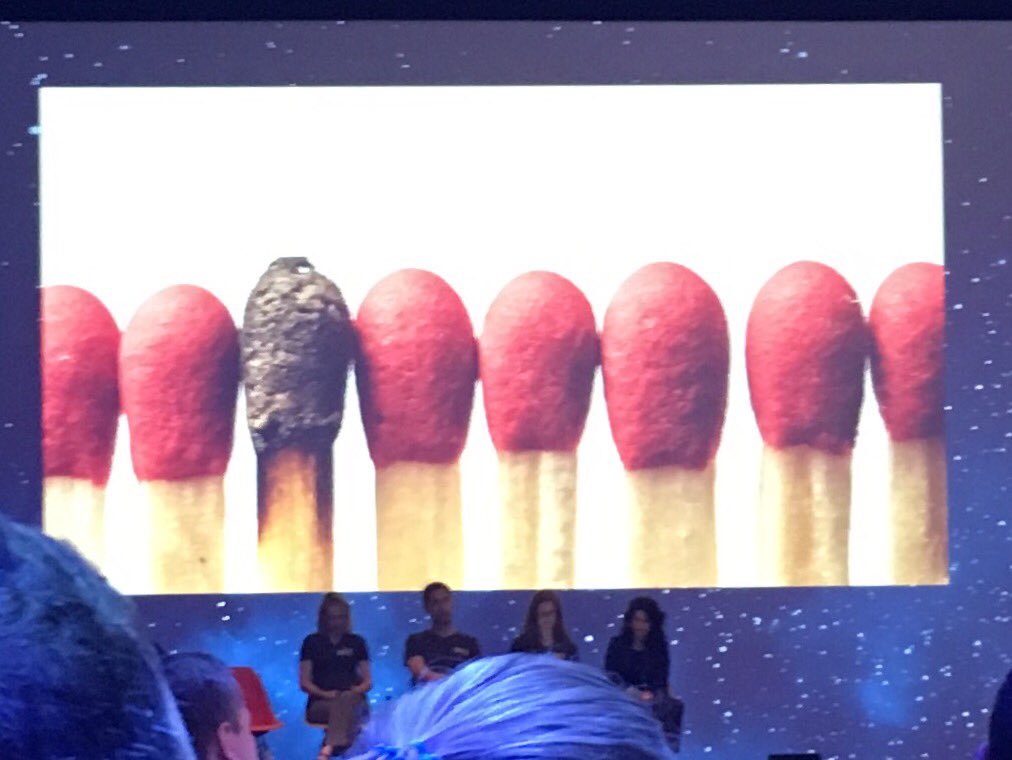
LIGHTING THE FLAME: CRITICAL CARE EDUCATION
Chair: Simon Carley
Panel: Jenny Rudolph, Walter Eppich, Chris Nickson, Victoria Brazil, Sandra Viggers, Daniel Cabrera
The morning however was worth the trek in. An inspiration panel of educationalists (new word for me) on the future of education in Critical Care. There is a Storify thread which you can follow here as otherwise my succinct points below won't do it justice.
How to Fail - Kevin Fong
Another new man crush! Anaesthetist/Astronaut Kevin spoke about failure. The old saying is true; it's not an option. Failure will always happen. We have to adapt to accept this and approach our safety mechanisms and responses to failure appropriately. Hypercompetence is a myth. Hubris is wrong. We have to have 'graceful failure' otherwise human factors fails and we will let out patient down. I also liked his point that maybe the only reason medical science began to see the heart as a pump was because mechanics had invented a pump and we had a frame of reference. Makes me wonder what fundamental point we're currently missing because we don't have that frame today.
Helping Without Harming - Jenny Rudolph
An inventive and entertaining talk. Rather than being annoyed at someone and thinking WTF think another WTF (What's Their Frame?) The hashtag #WTF2WTF is alive and kicking on Twitter and it will be interesting to see how this goes. More about fundamental-attribution bias. Thought provoking, something I will try.
The Global Refugee Crisis: Why it’s Critical that we Care - Vera Sistenich
The only talk to get a standing ovation. I can't do it justice, watch it at the SMACC website. The more people who watch the better.
How to Fail… Part Two - Martin Bromiley
We all know his late wife's story. How he does it I don't know but another great talk. A man with much to be angry about who actually chose to understand and help. His thoughts were inspiring on human factors:
This isn't a cop out but I genuinely couldn't do the last session featuring Martin Bromiley and James Piercy justice so please check it out on the Das SMACC site. Amazing human beings and it was a privilege to hear them. I hope I don't have to go through what they did but I hope I could always be as kind.
So that was Das SMACC. Personally I love FOAMed and it was great to be with like minded people in an amazing city. Berlin is an amazing mixture of beauty and horror and needs to be seen. What about SMACC? It is a bit cultish if I'm honest. I can see the point of some of its detractors pointing out the swearing, the hashtags, how something is either great or sh*t. And it has made 'celebrities' of medics - yes I know the irony as someone who blogs and records his voice in his spare time - which is something that may create challenges in the future. But I loved it. SMACC has challenged the old school. Conferences where someone stands at the front and talks with no engagement are thankfully dying out. It's been great to see the smart conferences adapt with workshops, social media and an open minded approach. 'Punk movements' like SMACC are the vehicle of such changes. I hope I will always be so open minded. The focus on the next generation and innovation was a pleasure to see as well. Danke Berlin. Danke Das SMACC.
- Jamie

Typed in the shadow of the Tempodrom here are some of my highlights from the second day of Das SMACC; a lot discussed in the podcast which will also be out in a bit. Sorry if this reads a bit like a stream of consciousness poem.

A MEETING OF THE TRIBES: INTER-PROFESSIONAL ISSUES IN CRITICAL CARE
What tribe are you? As you increase complexity you can increase the tribalism shown. If there a rite of passage you go through after which you know you belong? The flat culture is celebrated until it falls apart under conflict. The microaggression - 'just a nurse' needs to be avoided.
A common enemy (such as ITU) can help unite it encourages more tribalism. The consultant sets the tone of the shift but so does everyone in the team. Be aware of fundamental attribution bias and distinguish between behaviour and intention. We often criticise others based on their behaviour but praised ourselves for our intentions regardless of outcome or behaviour. Vulnerability and intention build teams. Be aware of your emotional intelligence and think who you want to be. Don't wage time fixing what doesn't work build on what does work. Think about your team reflexibility and how tribalism may affect your education culture. Beware of emotional contagion - how we behave transmits to others. Positive feedback is often vague whilst critical feedback is specific and we often forget the positive feedback compared to negative so more positive is needed so the student/colleague remembers.
Making Complex Problems Simple: Chris Hicks
A brilliant talk breaking down the management of a very complicated trauma call. A large process doesn't mean complex. Keeping it simple needs strategy. We make our habits and then our habits make us. We don't want any wild variances at the simple level. Four stages: Habit, Emergency Theory, Factor down problem, Limit variables.
Emergence theory creates complexity (this is how swallows appear to be flying in sequence - swarm behaviour). Three factors at play much like a swarm: Alignment. Separation. Cohesion - break you team down into sub teams: those dealing with airway, those on chest, those on pelvis etc.
Factor down from surface complexity e.g. look at airway problem, circulatory problem rather than whole massive problem.
Limit variables - eliminate steps, reduce team numbers, practice sim and increase engagement
Dream Big Plan Simple
The Future of Out-Of-Hospital Cardiac Arrest: Maaret Castren
50% of sudden cardiac risk had symptoms in preceding 4 weeks yet there is no risk prediction tool. Recommended the European Resus Academy - 10 steps to improve cardiac arrest survival.
Learning from Sim Part II: Critical Moments in the Emergency Department: Chris Hicks
Discussed emotional valence in simulation: if you feel an emotion in simulation you will better remember it when you feel that emotion for real i.e. anger or fear. Must practice good psychological health in simulation.
Finding the Needle in the Haystack: Paediatric Cardiac Disease: Michele Domico
Cardiac disease presents every other way than chest pain, murmur, cyanosis and hypoxia are obvious but far more common and vague are fatigue, failure to thrive, sepsis.
Children should not be fatigued, think if it adds up. Infection may unmask. Quiet tachypnoea can mean easily missed poor perfusion. Small children should not be quiet when you examine. Normal BP and HR does not mean good CO. Might have multiple presentations and have been given another diagnosis. Beware cognitive bias. Think heart in cases of repeat presentations.
Guts or Gadgets?… Prayers or Protocol?… Training or Tricks? - MJ Slabbert
Discussed the process of naturalistic decision making as she brilliantly went through a case of penetrative chest injury peri-arrest in the community. Do you go with protocol and RSI there knowing the BP will plummet and you'll have to do a thorocotomy in the community or scoop and run 5 minutes to hospital? Which is best?
16 Bits of Anaphylaxis - Daniel Cabrera
An outstanding presentation invoking Space Invaders.
Resuscitation for the Resuscitationist
Mass panel discussion here. No clear outcomes but some interesting areas of debate:
Vasoplegia e.g 130/7 - intravenous do not work
Preemptive CPR
? Use of Methylene blue
Refractory VF
Repositioning the pads
Or
Additional machine with 2nd set of pads with synchronized defib
Esmolol for refractory VF worth a try
Isoprenaline injection
Ketamine for semi-conscious patients during CPR
Encourage awake arrested patient to cough
When enough is enough-- close to 40 min of good quality CPR
Post resus temp control aiming 32-34C
Paralysis for temp control
Right, off to get the podcast out and then get to the party! Enjoy!
- Jamie

Just a few initial thoughts whilst the first day of Das SMACC is still free in my head!
Pre-Hospital Medicine: The Future is Now: Brian Burns
Trauma is a silent killer with 14,000 killed every day or 5 million a year. As a proud geek I fully approved of the demonstration of technology as a 'meerkat system' to predict severity, POCUS and point of care TEG with drones providing tailored blood products to the scene. Early day yes. Orwellian possibly. Exciting definitely.
Jonathan's Story: Jessica Mason
I'm always looking for new ways of teaching and found the approach by Jess Mason of using a patient story inspiring. She said "remember the story, remember the medicine" as she used the story of a patient of hers with sickle cell anaemia to make an important point: it is a terminal disease and should be treated as such; be kind with analgesia - opioids are the best.
Voices in my Head: Sarah Gray
Do you talk to yourself in the same way you would talk to a patient? Sarah talked about self compassion, an area of interest for me as my masters dissertation looks as mental health and resilience. This may be the subject of a future blog as she recommended the site selfcompassion.org as a window into our emotional health. Asked the audience to put their hand in the air and then lower it down if we knew someone who had died of suicide, suffered depression or self-harm. One hand out of 2500 was left in the air at the end... Don't burn out!
“Everything” at the End of Life: Alex Psirades
It's a fact that all medical students are trained in CPR but not in how to discuss DNAR. There were powerful reminders that as healthcare workers we all share the same ultimate fate of our patients: our mortality. Even with improvements in medicine the mortality rate in the 21st century remains the same as the 17th. Alex mentioned optimism bias and how as clinicians prognostication of terminally ill patients actually worsens as we know them more as people. He highlighted the HHHHHMM scale used in veterinary medicine which I think actually has some transferability to human patients.


The Problem with Physiology: Rinaldo Bellomo
"Today's medicine is tomorrow's derision" Rinaldo highlighted the problems of physiology with example discredited practices such as Early Goal Directed Therapy, replacing albumin, replacing Protein C or prophylactic craniotomy. More biases here - attribution bias & immediacy bias. That fluid bolus you gave to correct your patient's BP? In 20 minutes it will be back to baseline. Mad Physiology leads to Mad Medicine.
Four Tragic Dog Deaths: Lessons in Program Design and Development: Resa Lewiss
A good look at programme design with the four pillars I recognised from DREEAM: Clinical Excellence, Education, Research and Administration. Resa used the deaths of four of her childhood dogs as examples of how a project may die: Cancer - a slow, insidious killer such as a cultural or personnel issue, Homicide - someone outside comes along and pulls the plug, Suicide - something you do kills your project and Old Age - your project fails to adapt and grows old and gets passed by. Powerful and like all good presentations memorable.
Endocarditis will also f&*k you up: David Carr
Endocarditis. There is a 1% risk per year of endocarditis for patients with valve replacement. The risk is 1-2% in intravenous drug users. There thrombotic non-bacterial endocarditis: marantic endocarditis seen in malignancy and anti-phospholipid syndrome related endocarditis seen in lupus. 95% will have fever. 90% will have a murmur. To think of it as 'fever plus one'. Fever plus stroke in the young - usually MCA infarct - should make us think endocarditis. Fever plus back pain (osteomyelitis suggest haematalogical spread of the organisms which can also cause endocarditis). Fever plus heart failure (especially if there is no history of CCF - 'virgin' heart failure. Failure plus arrhythmia. (First degree heart block may be boring but suggests pervalvular abscess). Only 5% will have peripheral stigmata such as Janeway lesions or Osler's nodes - I'm going to have to change my teaching. Far more important is to look in their mouth, dental work in the preceding fortnight is suggestive and easier to identify than Roth's spots.
Plenty to discuss in the future. For now I hope you enjoy reading. Off to upload the podcast!
- Jamie

Take Aurally is off on holiday next week and this being Take Aurally it's going to be a FOAMed themed occasion!
SMACC (Social Media and Critical Care) is a health promotion charity. It is based on the philosophy of FOAM (Free Open Access Medical education – #FOAMed). DAS SMACC is being held at the Tempodrom, Berlin from 26th-29th June. For more information visit their website.
I'll be recording, photographing, blogging and tweeting from the conference and I'm looking forward to an inspirational few days! Hopefully see you there!
- Jamie

Thanks to @JamesPrattACP for pointing out this great video! Apologies if you're not a geek like me; ask your kids. It makes me wish we had someone waving red flags at us as we talk to patients.
How important are red flags to your practice? Despite the continuing negative press aimed at the NHS 111 service I think if we were on the phone hearing a patient describing the ''worst headache ever that came on quickly'' I very much doubt many of us would advise the patient to wait to see their GP. Red flags exist for a reason. They can point out the obvious as Watto is doing to Qui-Gon. Unlike Qui-Gon we should listen.
''Listen to your patient, he is telling you the diagnosis" - William Osler
I'd imagine every healthcare worker has stories of patients that act as a reminder to be humble and open minded. These cases can form our reflective practice, our teaching and help make us better at what we do if we handle them properly. We've all seen the horror stories often misrepresented in the press but if we follow red flags we can practice safely; it's not about fear it's about doing the best for our patient. It's also about being up to date. For example through safety alerts from the Royal College of Emergency Medicine or Trauma Audit and Research Network data I know I have changed my approach to elderly patients presenting with abdominal pain or a fall. On the other hand work such as the MACS decision rule challenges long held clinical convention that 'cardiac sounding chest pain' is always crushing, central and radiates to the left hand with pins and needles.
There is an interesting paper joint written by a conference of the Royal Collage of Physicians and British Geriatric Society which I recommend reading that takes a systems based approach to red flags. I think that's a very useful tactic when teaching history taking; by learning red flags and the reasons behind cardinal symptoms we improve our focused history taking and handovers.
I enjoy teaching on the Enhanced Clinical Skills course run by @JamesPrattACP on which I do a session on red flags and clinical bias. It is refreshing as someone who exists in the bubble of Emergency Medicine to see the perspective on red flags from community nurses in a variety of specialties; from general practice to psychiatry. Due to the sheer breadth of presentations in the community there are some great primary care orientated resources based on red flags. There's often reminders of how my work might have blunted my own perspective such as when I mention haemoptysis and the community based audience all diagnose cancer when pulmonary embolism was actually foremost in my Emergency Medicine biased mind!
In this session I discuss the inherent biases we all carry. Some can be unavoidable but we can and need to be aware of them; I use the example of 'the dress' for this as it also works as a good ice breaker.

The dress. It's white and gold by the way. Clearly.
We explore different sorts of biases through some, exaggerated, hypothetical scenarios. Yes, there's some cliche (the horse vs zebra conundrum is unavoidable) but I hope through the session to get our students to explore their own pre-conceived approaches to common clinical conditions as well as facing up to clinical decision making biases.

Whilst all important I find two in particular challenge us day to day.
Knowledge of potential biases as well as insight into our limitations helps make us safer in our practice. As best explained from former US Defence Secretary Donald Rumsfeld it's all about those unknown unknowns!
Here is a recording of my session on red flags and clinical biases recorded in front of an audience of community and hospital nurses. I have edited out some of the group work sessions for brevity.
- Jamie
"Attack ships on fire off the shoulder of Orion. I watched C-beams glitter in the dark near the Tannhäuser Gate. All those moments will be lost in time, like tears in rain. Time to die."
Blade Runner is one of my all time favourite films and I think this soliloquy by Roy Batty is one of the most beautiful pieces of improvisation ever put to film.
What does this have to do with FOAMed? Well the metaphor of memories being lost like tears in rain is used rather brilliantly by one of my education heroes Ross Fisher (@ffolliet). No matter how good the subject matter if the presentation is poor the message is lost. Like tears in rain. Through presentations and his own website Ross has helped place a focus on how we can improve the way we teach through the 'p cubed' approach.
I'm not going to repeat his work here other than to say if you teach or present anything about any topic you need to see his website and listen to his podcasts. You will learn and be inspired.
From a personal point of view I certainly was taught through 'death by PowerPoint' at medical school. Sadly, this was how I then attempted to teach once I became a fellow. Thankfully I was introduced to Ross's work by a former colleague @dominic_purnell. Needless to say, this has had a profound affect on how I teach now.
Interestingly, there is often some resistance from other colleagues primarily I think because of being used to teaching with PowerPoint as the sole focus - ''as a crutch'' - but if you view it as an aid and make yourself the focus of attention it is amazing what can happen.
No one can cover every topic in one session but we can inspire and enthuse. In this presentation I spoke in front of my fellow educators at DREEAM about p cubed and my own 'journey' in teaching. I also talk about some other useful technology such as Mentimeter, TweetDeck and QRS Codes which I might blog about separately another day. It is quite personal but I think shows how nearly 2 years of teaching has changed my approach. It also gave me a chance to reference James Bond (RIP Sir Roger), Indiana Jones, Sir David Attenborough, Robin Williams AND Ferris Bueller - not many presentations can do that!
Hope you enjoy my presentation which does use a lot of Ross's material (why reinvent the wheel?). Check our his website and podcasts. And watch Blade Runner if you haven't. It's amazing.
- Jamie